Ganesh M. Shankar, MD, PhD
Massachusetts General Hospital
Background
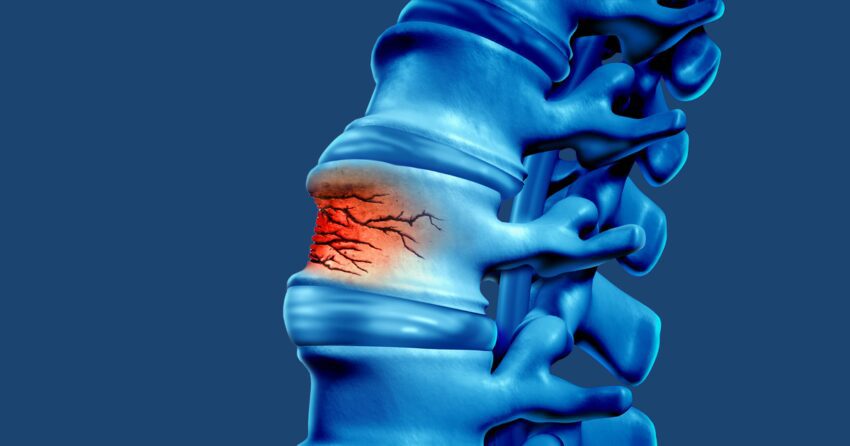
Osteoporotic vertebral body compression fractures (VCFs), or vertebral insufficiency fractures, occur when the density of the bone is insufficient to maintain its structural integrity in the setting of trauma or even minor events. VCFs most commonly occur in the lower half of the thoracic spine or upper half of the lumbar spine. They are accompanied by pain along the spine that occurs with activity or postural changes, roughly at the location of the fracture. These types of fractures are not commonly associated with symptoms of leg pain or weakness. Surprisingly, many fractures are “silent” because patients do not have any symptoms from them.
Risk Factors

One major risk factor for a VCF is low bone density, which is measured with a bone density scan. Other important risk factors are prolonged use of steroid medications, any history of prior fracture, or certain medical conditions such as hyperparathyroidism and chronic renal failure. They are frequently seen among post-menopausal females as the balance in maintaining skeletal mineralization is shifted away from deposition of new bone to increased bone turnover with the loss of estrogen. Approximately 20% of patients with a prior VCF will sustain another vertebral fracture over the following 12 months.
Evaluation
VCFs are evaluated with imaging studies to delineate the location of the fracture, the anatomy of the fracture, and impact on the spinal alignment (tendency to bend over). The impact of the fracture on spinal alignment is visualized by standing spine X-rays – either a focused image of the involved segment (thoracic or lumbar) or the entire spine (scoliosis view). These imaging studies will also provide more confidence that the VCF is a result of low bone density rather than an underlying pathology, such as a tumor. An MRI can help determine the age of the fracture and presence of pinching of the spinal cord or nerves which helps to plan the best course of treatment.
Management
When an osteoporotic VCF is diagnosed, there are two considerations for management – (1) addressing the symptoms and (2) reducing the risk of future insufficiency fractures.
Treating Symptoms
The acute symptoms are often managed well with acetaminophen and anti-inflammatory medications such as ibuprofen or naproxen, available over the counter. If the pain is severe, then a short course of opioid analgesics may be required. Calcitonin is a hormone normally secreted by the thyroid that reduces serum calcium by inhibiting cells that break down bone (osteoclasts). A recombinant form of calcitonin isolated from salmon can be administered subcutaneously or intranasally and has been demonstrated to reduce pain for the first 2-4 weeks following a VCF.
Intermittent use of a brace can also help reduce pain in the acute and subacute stages, but chronic long-term use can lead to atrophy of the paraspinal muscles from disuse. Similarly, to prevent deconditioning of these core muscles following a VCF, return to activity as tolerated and engagement in physical therapy, including consideration for aqua therapy, is encouraged.
Vertebral augmentation is where cement is injected into the broken vertebra to provide stability and rapid pain relief. This treatment is an excellent option for patients with an acute or subacute (<6 months) VCF who have ongoing discomfort that is refractory to analgesic therapy and activity modification. Two techniques are available. Vertebroplasty involves the injection of cement (polymethylmethacrylate) into the fractured vertebral body under X-ray control. Kyphoplasty has the additional use of a balloon to expand a cavity within the fracture with the goal of restoring vertebral body height and permitting a larger volume of cement.
These procedures are performed with sedation or general anesthesia. Vertebral augmentation has the highest likelihood of therapeutic benefit in patients with severe pain that is refractory to oral analgesics. The pain relief achieved in this timeframe can often facilitate engagement with core strengthening exercises and mobilization.
In patients with chronic pain from VCF, with discomfort lasting longer than 6-12 months, there should be consideration for repeat imaging by X-ray, CT, and MRI. The structural etiologies that can result in persistent pain include (1) VCF at a new level, (2) progressive kyphosis (hunchback) at the level of the fracture, and (3) compression of the neural elements at the level of the fracture. Depending on the findings of these updated imaging studies, patients with persistent pain can be considered for vertebral augmentation (if new acute/subacute fractures are identified), physical therapy (core strengthening), pain management for consideration of facet ablations, and possible surgical evaluation (if compression of the neural elements is suspected to be contributing to the ongoing discomfort). Surgical treatment is rarely warranted as poor bone quality is associated with many complications.
Reducing Future Fractures

To reduce the risk of future insufficiency VCFs, the underlying bone density will need to be addressed metabolically. The mechanism of these pharmacologic interventions is based on altering the physiology of bone maintenance – which is a constant balance of breaking down old bone and forming new bone. The use of medications is discussed in detail in the previous article. Medications to treat osteoporosis are very effective: bone density can increase up to 15% in one year and future fractures are reduced by 60%-75%. Patients older than 65 years with a fragility spinal fracture are candidates for medication treatment to prevent the next fracture. In addition, early treatment may lead to more rapid pain resolution.
Conclusion
In summary, the pillars of VCF treatment are in diagnostic imaging and pain management (oral analgesics, physical therapy, and vertebral augmentation). Treatment of underlying bone metabolic disorders will also need to be considered in this patient population. The vast majority of patients presenting with a VCF can be managed non-operatively with the central goal of restoring function and mobility.