A healthy spine is essential, and taking care of the 33 bones – the vertebrae – that make up your spinal column is critical to ensuring that your spine remains healthy and functions well as you age.
Osteoporosis is a medical condition characterized by the weakening of bones, which leads to a higher risk of bone fractures. It is sometimes called a “silent disease” because many people do not realize they have it until a fracture occurs, since there are no symptoms that prompt early evaluation.
This condition is particularly relevant to spine health because studies have demonstrated that fractures from osteoporosis occur most often in the spine and happen an estimated 1.5 million times a year.
Nevertheless, despite being so common, most people don’t fully understand the condition nor realize that osteoporosis is treatable and that most cases of osteoporosis-related fractures are completely preventable through the right treatment plan.
In this article, we explore the topics of bone health, osteoporosis and your spine.
- What is osteoporosis?
- What are the symptoms of osteoporosis?
- What are the causes of osteoporosis?
- What medications increase the risk of osteoporosis?
- Can spinal compression fractures be related to osteoporosis?
- What is osteopenia?
- Who is at risk for osteoporosis?
- Can you prevent osteoporosis?
- Can medical conditions worsen osteoporosis?
- How is osteoporosis diagnosed?
- How is osteoporosis treated?
- Are you at risk for osteoporosis?
- Bone health in children
What is osteoporosis?
Osteoporosis is a systemic condition characterized by the weakening and deterioration of the skeleton, which includes the spine. Having osteoporosis makes the bones more fragile and susceptible to fractures, which can cause compression fractures of the vertebrae, leading to back pain.
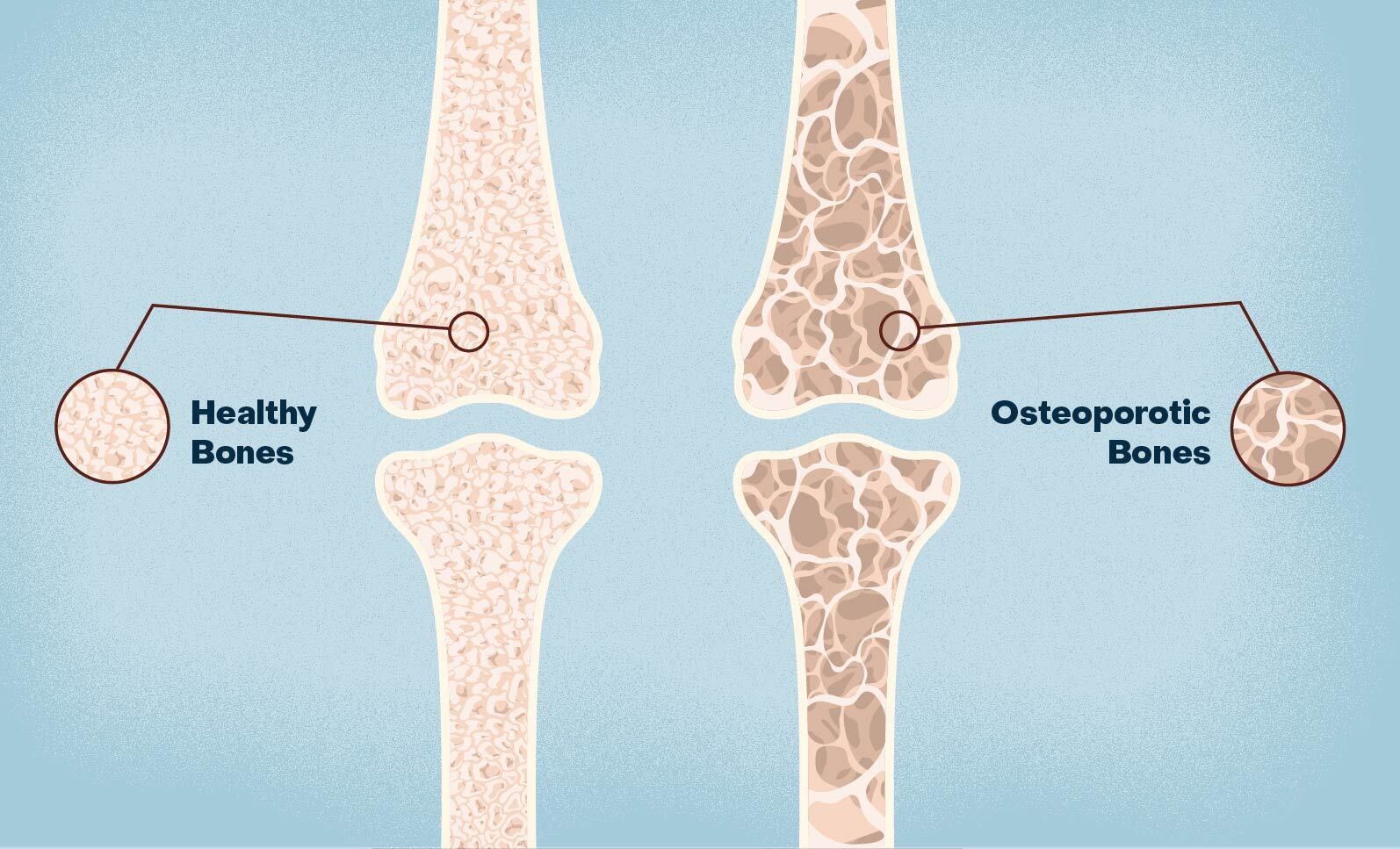
Healthy bones are dense and strong. Osteoporosis causes bone density and quality to deteriorate over time. As a result, the bones become porous and brittle, resembling a honeycomb-like structure under a microscope. Compromising the structure of bones is a set up for fractures.
Osteoporosis is often referred to as a “silent disease” because it typically progresses without any noticeable symptoms until a fracture occurs.
It is not common knowledge that bones are turning over constantly; they’re changing and evolving with motion, lifestyle and age. Over time, bone mass is weakened faster than it is strengthened. Your skeleton may be getting weaker and weaker, but you wouldn’t feel it – it’s not painful.
What are the symptoms of osteoporosis?
Osteoporosis may not cause noticeable symptoms in its early stages. In many cases, individuals with osteoporosis may not be aware of the condition until they experience a fracture or related symptoms. Some individuals may notice a loss of height compared to when they were younger, but chalk it up to the aging process rather than to poor bone health.
When symptoms do occur, they can include:
- Persistent back pain: The pain may occur in the middle or lower back and may worsen with movement or activities like lifting, bending, or twisting.
- Change in Posture: Osteoporosis-related fractures can lead to a change in posture, particularly an exaggerated rounding of the upper back. This altered posture is known as “dowager’s hump” and is more common in advanced cases.
- Limited Mobility: Severe cases of spinal osteoporosis can restrict an individual’s mobility and flexibility, making it challenging to perform daily activities or maintain an active lifestyle. If fractures have occurred, these often have devastating consequences and limit daily activities such as walking, bathing, and dressing.
What are the causes of osteoporosis?
There are many risk factors for developing osteoporosis, all of which are more pronounced with age. There are 2 main types of cells that affect bone density, the osteoblasts that build bone and the osteoclasts that break down bone. Before the third decade of life, the osteoblasts are hard at work building bone and we reach our peak bone mass during this time. As we grow older, the osteoclasts become the major player, breaking down bone, causing our bones to lose density and become more susceptible to fractures. This process affects both women and men but is more pronounced in postmenopausal women due to the added negative effect of hormonal changes.
Our diet and exposure to direct sunlight play a significant role in supporting our bones. Inadequate intake of calcium and Vitamin D leads to deficiencies in the vitamins and minerals necessary to strengthen bone. Getting enough of these nutrients when we are young helps to build up a “bank” for our bones to use in the future. Malnutrition is a risk factor for osteoporosis.
Lifestyle factors have a direct effect on our bone health. Living a sedentary lifestyle, smoking/vaping and drinking excessive alcohol are all behaviors that can weaken bone density and are considered risk factors for osteoporosis.
The role of genetics is important to understand. In addition to your genetic code dictating your size, gender, and race – which are important bone density factors – you may also inherit the propensity to develop osteoporosis from your parents, so it’s important to know your family history. If one of your parents has a history of a hip fracture, then your risk of osteoporosis is greater.
What medications increase the risk of osteoporosis?
Several medications and medical treatments can potentially weaken bone density. However, it’s important to note that the risk can vary depending on factors such as the type of medication, dosage, duration of treatment, and individual susceptibility.
- Corticosteroids: Long-term use of steroids like prednisone or cortisone is a significant risk factor for medication-induced osteoporosis. These medications suppress bone formation and impair calcium absorption.
- Seizure Medications: Some antiepileptic medications, including phenytoin, carbamazepine, and phenobarbital, can interfere with the metabolism of Vitamin D and calcium, leading to decreased bone density.
- Antidepressants: Selective serotonin reuptake inhibitors (SSRIs), such as fluoxetine and paroxetine, have been associated with a modest increase in fracture risk, possibly due to their impact on bone turnover.
- Proton Pump Inhibitors (PPIs): Long-term use of PPIs like omeprazole and esomeprazole, used to treat acid reflux and stomach ulcers, impair calcium absorption.
- Thyroid Hormone Replacement: Excessive thyroid hormone replacement in individuals with hypothyroidism can increase the risk of osteoporosis.
- Immunosuppressants: Some medications used to suppress the immune system, such as methotrexate and cyclosporine, may affect bone health when used long-term.
- Blood Thinners: Prolonged use of high-dose heparin and certain anticoagulants may contribute to bone loss.
- Chemotherapy: Some chemotherapy agents, particularly in high doses or when used in combination with other treatments, can have detrimental effects on bone density.
Can spinal compression fractures be related to osteoporosis?
Yes, compression fractures in the spine are a common consequence of osteoporosis. Often, people with osteoporosis do not know they have the condition until they experience a fracture.
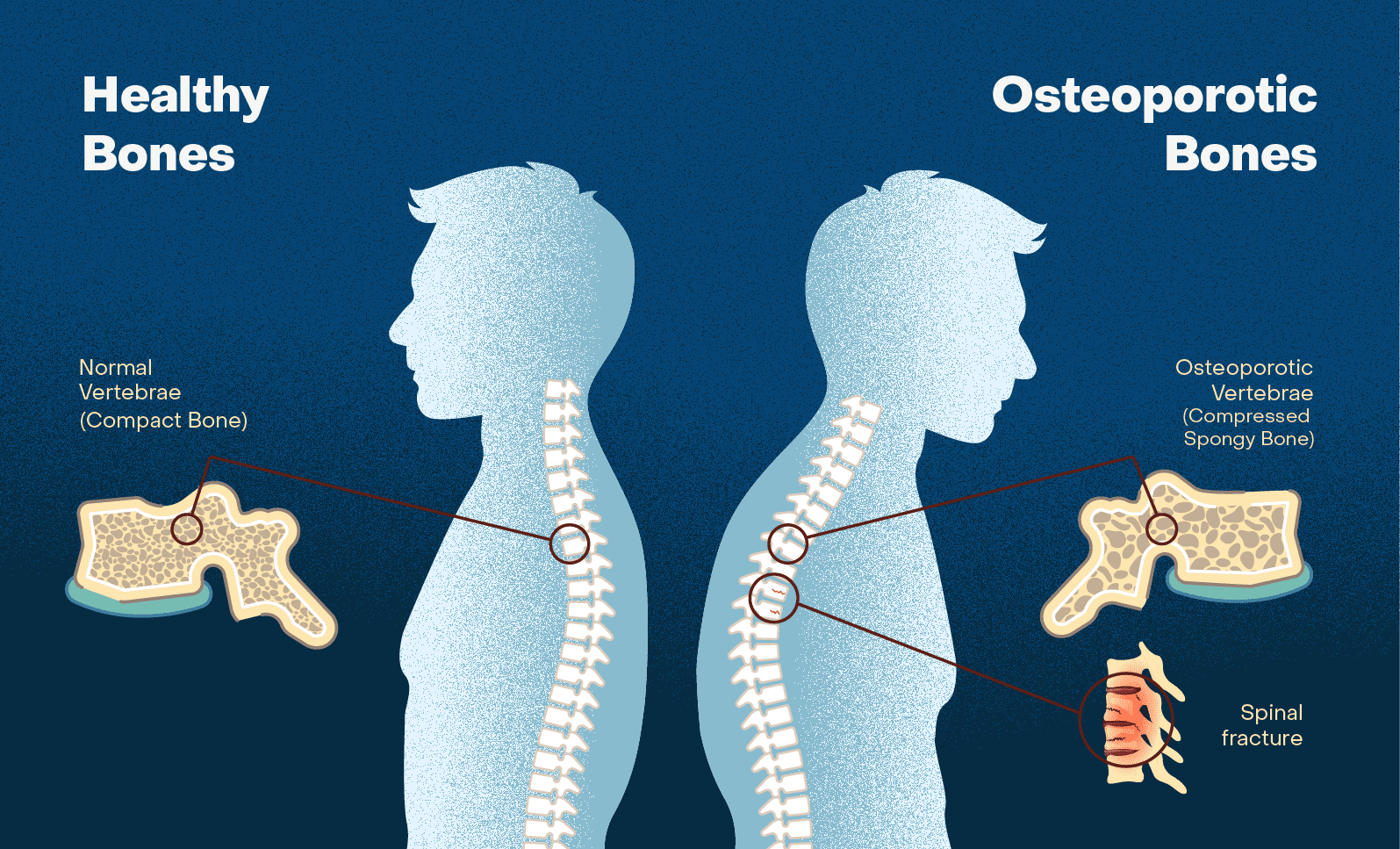
When osteoporosis causes compression fractures in the spine, the bones of the spine become so fragile that even normal everyday activities, such as bending, lifting, or coughing, can exert damaging pressure on the vertebrae. These fractures typically occur in the front (anterior) part of the vertebral body, causing it to collapse or compress.
Compression fractures can be painful and may cause localized back pain, which can range from mild to severe. Some individuals may also experience nerve-related symptoms, such as numbness, tingling, or weakness, if the fractured vertebrae put pressure on nearby nerves.
What is osteopenia?
Osteopenia is a lesser-known term than osteoporosis, but just as important to understand. Osteopenia is a medical condition characterized by bone density that is lower than normal but not as severe as osteoporosis – essentially, osteopenia is a milder form of bone weakening.
The main difference between osteopenia and osteoporosis is the degree of bone density loss and the associated fracture risk. While individuals with osteopenia have lower bone density than normal, they are not as prone to fractures as those with osteoporosis. Osteopenia can serve as a warning sign or a precursor to osteoporosis. It is important to identify and manage osteopenia to prevent further bone density loss and reduce the risk of developing osteoporosis and osteoporosis-related fractures.
Who is at risk for osteoporosis?
There are a number of different factors that can put you at risk for developing osteoporosis, including age, lifestyle, weight and medications. Doctors typically divide risk factors into two main categories, modifiable risk and non-modifiable risk:
Modifiable Risks:
There are several modifiable risk factors that you can control through lifestyle changes and medical interventions. These modifiable risk factors include:
- Smoking/vaping: Smoking has a very high association with osteoporosis. Tobacco smoke is made up of more than 7,000 chemicals, including over 70 known to cause cancer (carcinogens), and they can contribute to bone weakening. Vaping constituents have been linked to poor bone health.
- Diet: A diet lacking in calcium and Vitamin D, but full of excessive sugar, salt, and caffeine puts you at higher risk for osteoporosis.
- Physical Activity: Exercise is one of the most important things you can do for your bones and your spine. A sedentary lifestyle will not stimulate your bones to strengthen, increasing the risk of osteoporosis. This is why astronauts in space, who are not stimulating their bones, lose bone mass.
- Alcohol Consumption: Alcohol affects your liver, which regulates the metabolism of Vitamin D and produces important proteins related to bone health.
- Medications: Many medications, such as corticosteroids, could have a negative impact on bone health. While you may not be able to avoid the need for these medications, you must be aware of their bone effects and take measures to counter them.
- Caffeine: Excessive caffeine intake (more than two cups of coffee a day) may lead to negative effects on bone health. High caffeine consumption can interfere with calcium absorption in the intestines, which can affect calcium balance in the body and potentially lead to decreased bone density over time.
Non-Modifiable Risks:
Age and genetics are the two top non-modifiable risks for osteoporosis. It is a common misconception that osteoporosis is only something to think about when you’re older. The human body adds calcium to our skeletons to achieve peak bone mass by about 30 years old; then we start to lose calcium and break down bone at an increasing rate over time. So, our bones are becoming weaker as we age.
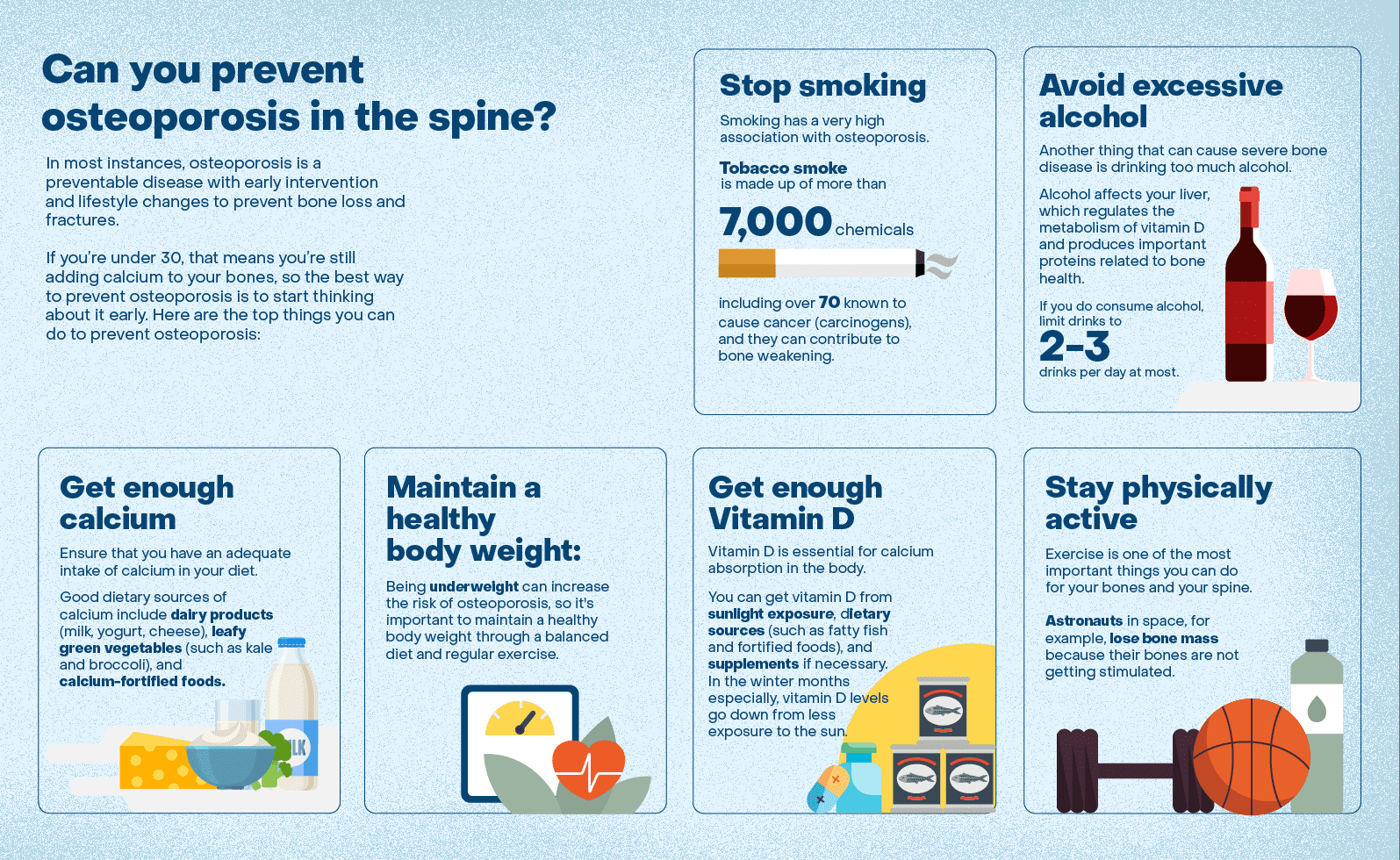
Can you prevent osteoporosis?
Osteoporosis is a treatable disease and may even be preventable with early intervention and lifestyle changes to prevent bone loss and fractures.
It is imperative to start thinking about bone health when you’re young. The bone bank of the skeleton is like an annuity program – you need to put calcium in when you’re young to be able to withdraw it as you get older with minimal consequences.
If you’re under 30, that means you’re still adding calcium to your bones, so the best way to prevent osteoporosis is to start thinking about it now. Here are the top things you can do to prevent osteoporosis:
- Stop smoking/vaping. Quitting nicotine reduces your risk of osteoporosis.
- Avoid excessive alcohol. If you do consume alcohol, limit drinks to 2-3 drinks per day at most.
- Get enough calcium: Ensure that you have an adequate intake of calcium in your diet. Good dietary sources of calcium include dairy products (milk, yogurt, cheese), leafy green vegetables (such as kale and broccoli), and calcium-fortified foods.
- Maintain a healthy body weight: Being underweight can increase the risk of osteoporosis, so it’s important to maintain a healthy body weight through a balanced diet and regular exercise.
- Get enough Vitamin D: You can get Vitamin D from sunlight exposure, dietary sources (such as fatty fish and fortified foods), and supplements if necessary. In the winter months especially, Vitamin D levels go down from less exposure to the sun. Your doctor can screen for low levels of Vitamin D through routine bloodwork.
- Stay physically active: Include weight-bearing exercises into your routine. This can be walking, jogging or strength training. Aim for at least 150 minutes of moderate-intensity exercise each week.
It’s also important to note that osteoporosis can be genetic. Some people are predisposed to having it. If a parent has had bone fractures, you should start proactive lifestyle changes much earlier.
Can medical conditions worsen osteoporosis?
Several medical conditions and illnesses can accelerate the development or progression of osteoporosis. These conditions may either directly affect bone health or lead to changes in hormones, nutrition, or medications that can weaken bones. Some of the illnesses and factors that can contribute to osteoporosis include:
- Hormonal disorders: Conditions such as hyperthyroidism (overactive thyroid), hyperparathyroidism (overactive parathyroid glands), and Cushing’s syndrome (excess cortisol production) can disrupt the balance of hormones in the body, negatively impacting bone density.
- Gastrointestinal disorders: Inflammatory bowel disease (IBD), celiac disease, and certain surgical procedures that affect nutrient absorption in the gut can lead to calcium and Vitamin D deficiencies, which are essential for bone health.
- Chronic kidney disease: Kidney disease can affect the body’s ability to regulate calcium and phosphorus levels, leading to bone problems.
- Eating disorders: Anorexia nervosa and bulimia nervosa can result in nutritional deficiencies, particularly calcium and Vitamin D, which can weaken bones.
- Chronic liver disease: Liver conditions, such as primary biliary cirrhosis and chronic hepatitis, can impact nutrient absorption and metabolism, affecting bone health.
- Multiple myeloma: This cancer of the plasma cells in the bone marrow can weaken bones and increase the risk of fractures.
- Hormone-related treatments: Certain cancer treatments, like hormonal therapy for breast or prostate cancer, can reduce estrogen or testosterone levels, leading to bone loss.
- Long-term use of certain medications: Prolonged use of medications such as glucocorticoids (steroids), anticonvulsants, and some proton pump inhibitors (PPIs) can increase the risk of osteoporosis.
How is osteoporosis diagnosed?
Bone density testing is the most definitive way to diagnose osteoporosis and assess bone health. The most commonly used test is a dual-energy X-ray absorptiometry (DXA or DEXA) scan. Radiation levels are extremely minimal (far lower than a CT scan, which can also measure bone density), so you don’t have to worry about radiation exposure.
This test measures the density of your bones, typically at the hip and spine, and provides a T-score, which compares your bone density to that of a healthy young adult. The results are used to determine your bone health status.
Based on your T-score, your bone health is classified as follows:
- Normal: T-score above -1.0
- Osteopenia (low bone density): T-score between -1.0 and -2.5
- Osteoporosis (very low bone density): T-score -2.5 or lower
These tests can provide a more accurate assessment of bone health than blood calcium levels. A person can have normal blood calcium levels but still be at risk for osteoporosis.
Why is that? Blood calcium levels are tightly regulated by the body, and the body maintains a stable calcium concentration in the blood by using calcium from the bones when necessary. So, even if your blood calcium levels are within the normal range in your lab work – which is just a snapshot of your calcium – your bones can still be losing calcium and becoming less dense, leading to osteoporosis.
Everyone should request a DEXA scan from their doctor if they’re over 50 or if they have a family history of osteoporosis. It serves as a baseline to compare to as you age over time. Multiple data points over time are much better at revealing patterns and predicting the future than one data point in time.
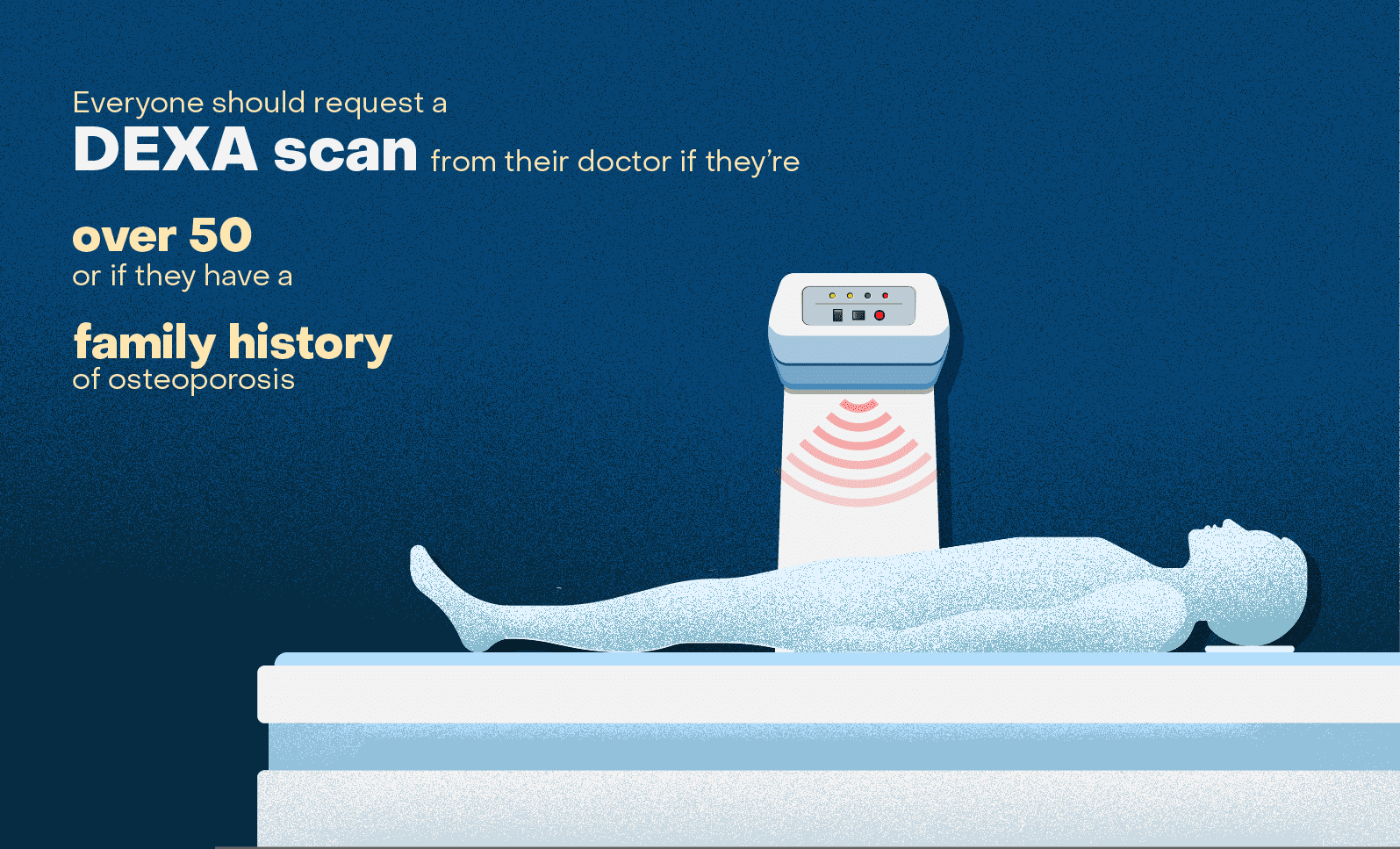
In many cases, health insurance plans, including Medicare, will cover DEXA scans for the diagnosis and monitoring of osteoporosis. However, coverage can vary depending on your insurance provider, the specific plan you have, and your risk factors.
Standard X-rays are not typically used as the primary method to diagnose osteoporosis because they do not provide a direct measurement of bone density. Instead, X-rays are more useful for identifying fractures or complications related to osteoporosis rather than assessing bone density. However, X-rays can indirectly indicate the presence of osteoporosis in certain situations.
Individuals with osteoporosis may require specialized postoperative care and medications to support bone health and minimize the risk of fractures.
Disc replacement technology has advanced tremendously in the field of spine surgery and is a type of motion-preserving spine surgery that is performed in place of a fusion. This procedure is not an option for patients with osteoporosis because the weak bones are unable to properly support the motion-preserving implants.
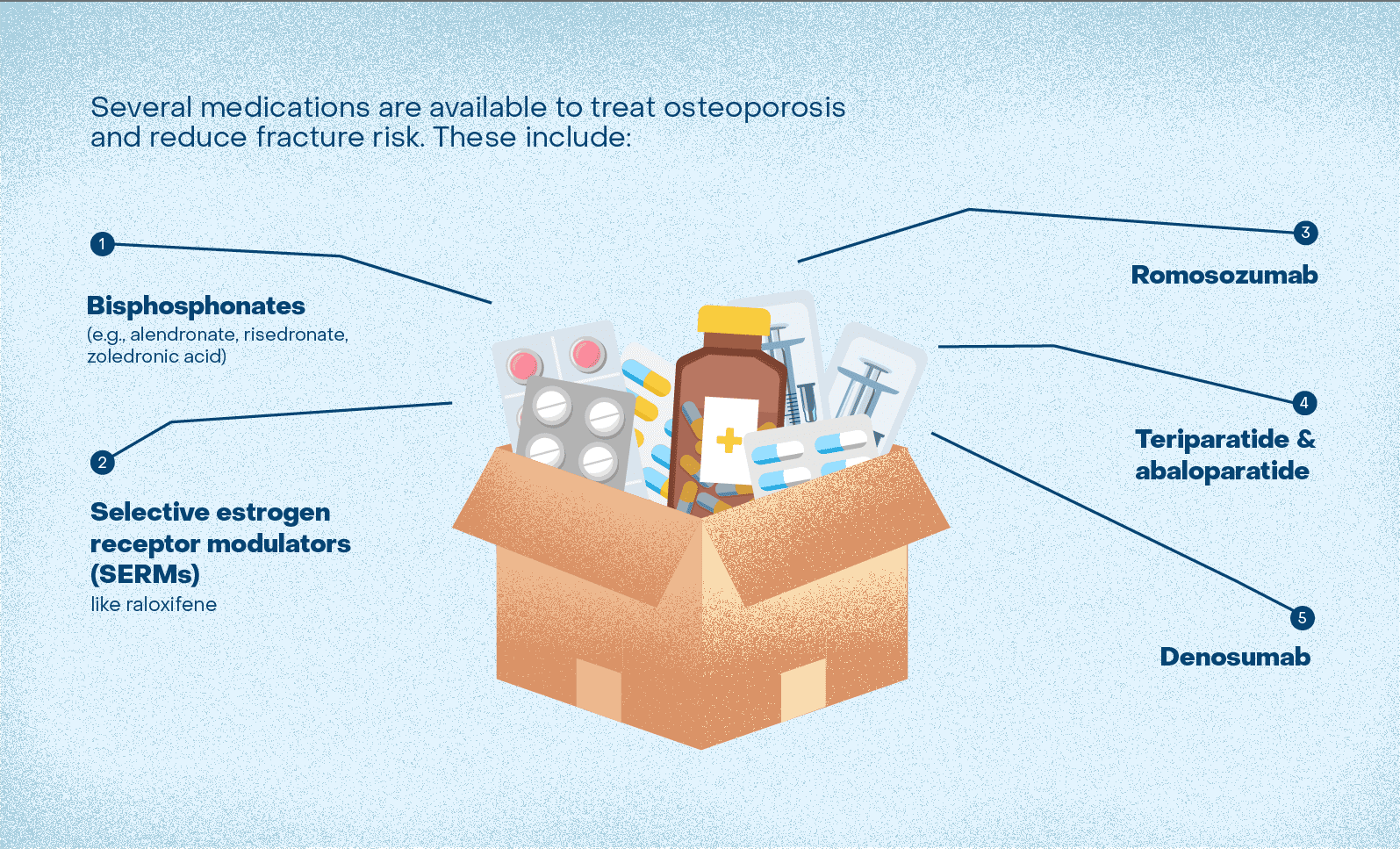
How is osteoporosis treated? Can osteoporosis be reversed?
While osteoporosis of the spine cannot be completely reversed, with proper treatment and lifestyle changes, it is possible to slow down the progression of the condition, increase bone density, and reduce the risk of fractures.
The best way to treat osteoporosis, first and foremost, is to make the same kind of lifestyle changes that prevent osteoporosis in the first place.
This includes exercising, eating a diet rich in calcium and Vitamin D, quitting smoking and avoiding alcohol. It also may include supplementing with calcium or Vitamin D.
Several medications are available to treat osteoporosis and reduce fracture risk. These include:
- Bisphosphonates (e.g., alendronate, risedronate, zoledronic acid)
- Selective estrogen receptor modulators (SERMs) like raloxifene
- Denosumab
- Teriparatide and abaloparatide
- Romosozumab
Discuss these medication options with your healthcare provider if you have osteoporosis or have sustained a low-energy fracture and meet the criteria for osteoporosis.
Are you at risk for osteoporosis?
Early detection and intervention are crucial in managing osteoporosis effectively and reducing the risk of complications.
Start by scheduling an appointment with your primary care physician. They can assess your medical history, risk factors, and symptoms related to bone health. They can also order appropriate tests, like a DEXA scan, or refer you to a specialist if necessary.
Depending on the severity of your condition and the results of the bone density test, your primary care doctor may refer you to a specialist, such as an endocrinologist, rheumatologist, or orthopedic surgeon, for further evaluation and management. These specialists have expertise in managing bone and musculoskeletal conditions.
Bone health is an evolving field and centers are increasing around the country, including places where people can go to get their bone health checked.
Doctors like Dr. Thomas Schuler, MD, FACS, of the Virginia Spine Institute; Dr. John Dimar II, MD, of Norton Leatherman Spine in Louisville, Kentucky; and Dr. Brandon Carlson, MD, MPH, of the University of Kansas Medical Center, who all participated in the National Spine Health Foundation’s Spine Talk on Osteoporosis and the Spine, are advocating for greater bone health awareness and patient resources.
Bone health in children
Bone health is important for people of all ages, including children. Healthy bones in childhood provide a strong foundation for lifelong bone health.
Parents should make sure that kids are getting enough calcium and Vitamin D in their diet and by getting enough sunlight. Focus on dairy products, leafy green vegetables, nuts and seeds, and fatty fish, like salmon. Some breakfast cereals and other foods are also fortified with calcium and Vitamin D.
Avoid sugary beverages, like soda, which can decrease calcium absorption. Encouraging water and milk as primary beverage options is beneficial for bone health.
Make sure kids are getting enough physical activity and regular checkups. Bones become stronger when they are stimulated by weight-bearing activities, another reason to get those kids off the electronics and outside.
Additionally, bone density is important in spinal deformity, like in scoliosis. Nearly 1/3 of these pediatric patients have osteopenia (low bone density). Low bone density can have significant effects on scoliosis treatment regardless of whether treatment includes a brace or surgery. Organizations like the Setting Scoliosis Straight Foundation (SSSF) are dedicated to researching spine and bone health for pediatric patients.
Conclusion
Your spine health matters. Your bone health matters. There are things you can do, starting now, to prevent problems down the road.
Pay attention to your diet: make sure you’re getting enough calcium and avoiding things like smoking that leach calcium from your body.
Pay attention to your mobility: Optimize your mobility by exercising several times a week, whether walking, lifting weights or doing another kind of exercise you enjoy.
Find out about your family history. If you have a family history of osteoporosis, or are an older adult, get a DEXA scan.
There is hope for people with osteoporosis. Advancements in medicine are being made every day. While prevention is always the best medicine, there are treatments for low bone density and ways to improve your spine health.