Introduction
Osteoporosis is a common condition associated with decreased bone mineral density and other structural changes in bone that reduce bone strength, which increase the chance of a fracture. Approximately 25%-30% of patients over the age of 50 years undergoing spine surgery have osteoporosis. Osteoporosis can be diagnosed based on DXA testing, fracture history, or when high fracture risk is present. DXA is commonly used to measure bone mineral density and when results (reported as a T-score) are less than -2.5, osteoporosis is present. Patients who sustain hip or spine fractures after the age of 50 years are also considered osteoporotic. In addition, osteoporosis is present if your fracture risk is high. One online tool to measure this risk is the FRAX 10-year risk calculator. Identifying, assessing, and optimizing risk factors to be better prepared for spine surgery will be explored in this article.

Bone Health & Elective Surgery
Bone health is very important to the results of spine surgery. Spine surgery typically removes some bone structure, potentially weakening the bone, which can lead to complications and need for further surgery. In addition, many cases involve the use of screws and cages that may loosen when the bone quality is poor. If fusion is performed, then a complex healing process occurs that may not be as robust when osteoporosis is present. Vitamin D helps build strong bones, even in adults, and is deficient in the majority of spine surgery patients. To emphasize the importance of bone health, one study from the Mayo clinic showed that 50% of patients with osteoporosis undergoing spinal fusion surgery developed bone-related complications, including screw loosening, vertebral fracture, failure of bone healing, and need for revision surgery. The good news is that medical treatment can improve bone quality, and treatment has been shown to improve outcomes and reduce complications. How do you know if you need treatment?
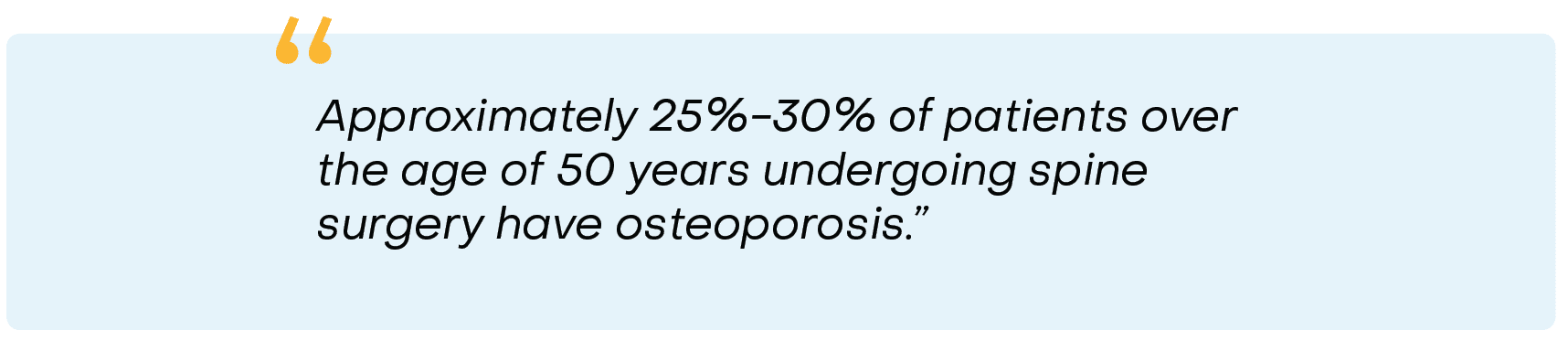
Know Your Risk Factors
Risk factors can help identify the presence of poor bone health and the need for treatment. The most common risks include older age, female gender, exposure to bone-harming medications and other toxins, sedentary lifestyle, fracture history, parental family history of hip fracture, certain comorbidities such as diabetes, hyperparathyroidism, chronic kidney disease, inflammatory arthritis, and low bone mass as measured on DXA. See Table 1. If you have been diagnosed with osteoporosis or have been treated for osteoporosis with medication, then you are at risk for complications after spine surgery.
Assessing Fracture Risk
A method used to calculate your risk and the need for medication is the Fracture Risk Assessment Tool or FRAX. This determines your risk for a hip fracture and a major osteoporotic fracture. The FRAX calculator is free to anyone and can be found by searching the web for “FRAX” or going to https://frax.shef.ac.uk/frax/index.aspx for the traditional version or www.FRAXplus.org to experience the updated version.
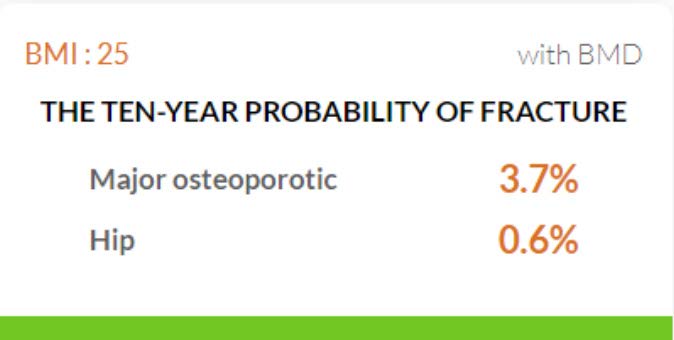
You will complete a short questionnaire that includes your region of the world and country, the presence or absence of 11 common risk factors, and your DXA results if available (otherwise leave blank). The output (see FRAX example) of the FRAX is the 10-year risk of a major osteoporotic and hip fracture. You are considered at high risk if your FRAX shows a hip fracture risk > 3% and major osteoporotic fracture risk > 20%; these are the thresholds to consider medical treatment.
Classify Your Bone Health

Bone disease is classified as low risk, high risk, and very high risk. It is important that adult men and women understand where they are currently at on this spectrum and monitor changes over time.
Low-risk patients have:
- No history of recent fractures
- T-score > -2.5 on DXA
- Low probability of fracture on FRAX
High-risk patients have:
- A history of a hip or spine fracture since age 50 years
- T-score < -2.5 on DXA
- 10-year probability of osteoporotic fracture > 20% on FRAX
Very high-risk patients have:
- A recent hip/spine fracture
- Multiple fractures
- Fractures while under treatment for osteoporosis
- Very low T-score < -3.0 on DXA
- High probability of fracture risk > 30% on FRAX
Pre-Surgical Bone Health Optimization
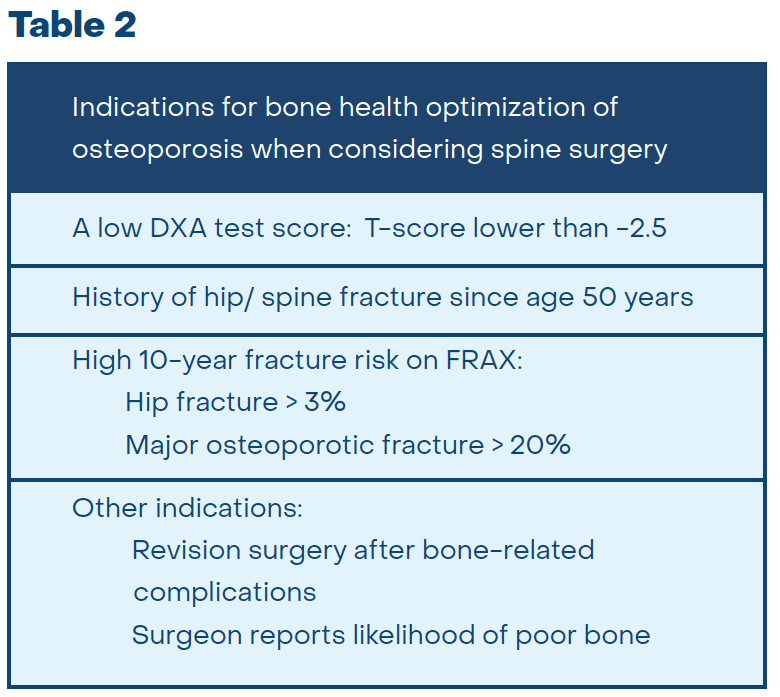
In some instances, optimizing bone health should be performed before and after surgery. Patients who are at high risk meet criteria for medical treatment of osteoporosis. See Table 2 for a list of indications to treat osteoporosis when considering spine surgery. Medical treatment for all patients should include 2000-5000 IU of daily Vitamin D3 and 1000-1200 mg of calcium in the diet or with supplements. If you meet criteria, prescription medication treatment can be initiated by the surgeon’s office or by a bone health specialist. The preferred medication would be an injectable bone-forming drug. These medications rapidly increase bone density, bone strength, and new bone formation within 2-3 months. Not all insurers will cover these medications and there are other effective medications that can be used.
A surgical delay to build your bone may be indicated if possible. The delay is usually 3 months but can be longer in cases where osteoporosis is severe or the surgery is very complex. This should be discussed with the surgeon and bone health team. If a delay is not possible, then medical treatment can occur after surgery.
Conclusion

Poor bone health is more common than you may think. You should consider your bone health prior to spinal surgery, as weak or brittle bone leads to complications and further surgery. Your fracture risk should be calculated and you should ask if a DXA test to measure your bone density is indicated. If you are at high or very high risk, then medical management should be considered.