By Thomas C. Schuler, MD, Virginia Spine Institute
This was the President’s Note from the Spring 2023 Spine Health Journal.
The phrase “you need a spine surgery” scares most people. Fortunately, through the development of modern techniques and technologies, today’s spine surgeons can vastly improve their patient’s quality of life with surgery. The artificial disc is one of these technologies benefiting patients suffering from debilitating neck or back problems by allowing them to regain their full and active lives after surgery. Historically, if someone suffered from disabling neck or back pain related to severe disc degeneration, the best treatment available was to remove the bad disc and fuse one bone (vertebra) to the next one. Over the past several decades we have developed better fusion techniques, but most exciting has been the development of the disc replacement (non-fusion) option. Fast forward to today and the use of artificial discs in the spine has vastly improved results for so many patients. Spine surgeons can remove a painful, degenerative, and/or herniated disc and replace it (disc replacement) with a new motion preserving device that keeps one functioning without debilitating pain.
Let’s review the anatomy of the spine to understand the application of disc replacement surgery:
- The spine is composed of a column of bones (vertebrae) which are connected to each other via discs.
- The disc is a strong ligamentous structure allowing for distraction, compression, flexion, extension, side bending, and rotational movements. The discs can function properly when these motions are preserved.
- There are two small joints (facet joints) in the back of the spine at each disc level.
- Together, the large disc in the front and facet joints in the back make up a 3-joint complex known as a motion segment.
When we perform an artificial disc replacement, we remove the damaged disc in the front and put a synthetic device in its place, which allows the motion of that 3-joint complex to be restored. This concept is very similar to a hip replacement surgery; however, in the spine we must consider the health of the facet joints. Think of a spinal motion segment as a tricycle. We can replace the big wheel in the front (the disc) but rely on the two small wheels (facet joints) in the back to be functioning. If the facet joints are reasonably healthy, then replacing the big disc in the front with an artificial disc allows us to preserve motion, restore function, and eliminate pain. Patient happiness often follows.
Artificial discs have been used very successfully over the past two decades and are now a standard of care. Despite this, insurance companies have been slow to accept this newer technology, even though the benefits have been well-proven in clinical trials as well as in practice. Ultimately, for patients to have access to new technology such as disc replacements, insurance companies must agree to pay for it. Unfortunately, many insurance companies often claim something is “experimental” even though it is not. This enables them to deny care and prevent access to these life-improving technologies. Furthermore, it is critical to understand that when a company develops a new product, FDA clearance must be obtained to distribute it in the US market. Many insurance companies further limit access to these implants by claiming that any scenario of use outside of the clinically narrow FDA trial is also “experimental.” As clinicians, we know that there are many clinical scenarios that would also benefit from these new technologies, but were not included in the FDA trial. Thankfully, FDA indications do not prevent surgeons from expanding the use of technologies beyond those initial limits, which ultimately allows surgeons to help more of their patients.
For example, postural problems such as forward flexed spines (kyphosis) were not included in the FDA trials of disc replacement implants. As a result, there is belief that artificial discs are contraindicated in cases of kyphosis. Just because certain indications were not tested in the original FDA studies does not mean other indications won’t work as well. Those of us proficient in artificial disc replacement have been successfully expanding the use of these implants by using our scientific knowledge and intuition to best benefit our patients. This means that the patients who undergo surgery for these expanded indications often have much better results than their traditionally fused counterparts. Cervical kyphosis is not an absolute contraindication to disc replacement technology, despite what some insurance companies say.
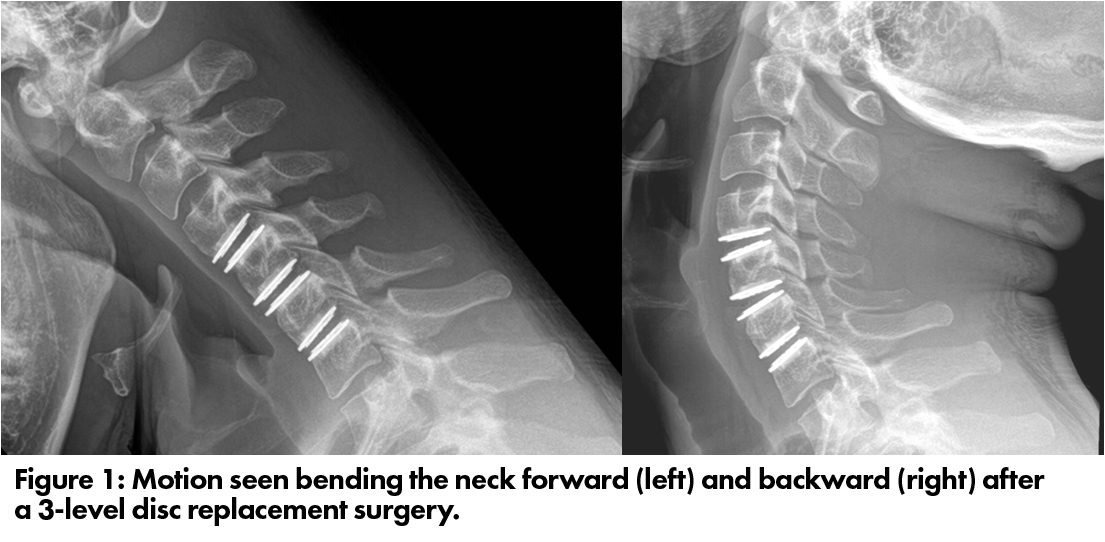
The long-term follow-up of the initial disc replacement clinical trials showed that while patients with fusions did well, those with disc replacements did better. None of the original trials looked at three- and four-level disc replacement cases, but it just stands to reason that in appropriately selected patients, a three- or four-level disc replacement procedure would produce even better results than a three- or four-level fusion. The logic is simple: if fusing the spine causes loss of motion through the fused levels thereby increasing stress at the adjacent levels, then preserving motion at as many levels as possible will produce a superior result, as the original trial demonstrated (figure 1).
The essential take away point is that when we can preserve motion, we should be doing that. When stabilization is required, then fusion is still a good operation. Sometimes we even combine these technologies, where we fuse the most unstable or degenerative level and then perform replacements at the other levels, still producing excellent clinical results compared to a fusion-only procedure. The great news is that through modern technological evolution, enhanced surgical techniques, and improved physician knowledge, we are better at restoring our patients to full and active lifestyles with the least short- and long-term problems. Patients do not need to fear modern spinal surgery performed by their trusted spine surgeons. In 2023, we should embrace all the amazing medical miracles that we have to restore and improve lives with spine surgery.



