What is Minimally Invasive Surgery?
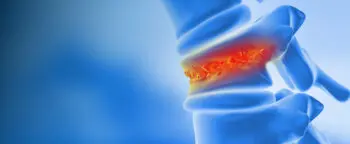
Minimally invasive surgery (MIS) is a revolutionary approach in modern medicine, particularly in spine care.
During the National Spine Health Foundation’s Spine-Talks, Dr. Rita Roy and experts Dr. Mike Wang, Dr. Frank Phillips, Dr. Neil Anand, and Dr. Sheeraz Quereshi share their insights about MIS. It focuses on achieving the desired results with the least disruption to the body. Unlike traditional surgeries that require large incisions and extensive muscle dissection, MIS utilizes advanced techniques and technologies—such as robotic assistance and specialized tools—to access the spine through small incisions and natural tissue planes. This approach minimizes collateral damage to surrounding muscles and tissues, reducing postoperative pain, recovery time, and complications.
As experts in the field emphasize, MIS is not just about smaller scars; it’s a philosophy of precision and preservation, ensuring that patients receive effective treatment while protecting their body’s structural integrity. By combining cutting-edge technology with patient-centered care, MIS has become a transformative option for those in need of spine surgery.
What is the Purpose of Medical Imaging in Spine Surgery?
Medical imaging plays a crucial role in spine surgery by serving as both a diagnostic tool and a roadmap for surgical planning. Techniques like x-rays, CT scans, and MRIs provide complementary insights into the spine’s structure and function, helping surgeons identify the pathology and correlate it with the patient’s symptoms.

Imaging helps surgeons determine the most effective approach—whether minimally invasive or traditional—to address the issue with minimal collateral damage.
However, imaging must be interpreted within the context of the patient’s needs and goals. Over-reliance on imaging can lead to unnecessary treatments, so the findings must align with clinical symptoms to ensure appropriate care.
Additionally, imaging assists in creating a precise surgical plan. It can be imagined as a 3D GPS, guiding surgeons to address the problem effectively while minimizing intervention. Ultimately, medical imaging is a vital tool that enables spine surgeons to diagnose accurately, plan meticulously, and tailor treatments to achieve the best outcomes for their patients.
What Do Patients Need to Know / Discuss with their Surgeon?
When considering spine surgery, it is imperative for patients to engage in informed, collaborative discussions with their surgeon to ensure optimal outcomes.
The first priority is establishing clear goals and expectations—identifying the symptoms to be addressed and determining whether surgery aligns with those objectives. Patients should thoroughly explore their surgical options, recognizing that procedures vary significantly in scope, intent, and technique, each with its unique advantages and potential drawbacks.

It is also beneficial to inquire about the scientific evidence supporting a recommended procedure, as not all techniques are equally substantiated by rigorous research.
Selecting the right surgeon is equally critical. Trust and comfort in the surgeon-patient relationship are key to effective care. Shared decision-making is important, too, as spine surgery often involves carefully balancing the patient’s individual needs, lifestyle considerations, and long-term health goals.
By educating themselves, asking insightful questions, and partnering with a qualified and experienced surgeon, patients can navigate their surgical journey with confidence and achieve the best possible results.
What Should Patients Ask about Minimally Invasive Surgery?
When discussing minimally invasive surgery with a surgeon, patients should focus on understanding the surgeon’s experience, philosophy, and commitment to their care journey.
Asking about the number of procedures a surgeon has performed and their familiarity with the proposed technique is both reasonable and essential.

Surgeons should openly share their experience and, when appropriate, direct patients to speak with others who have undergone similar procedures to gain a firsthand perspective.
Trust is fundamental; patients should feel comfortable with their surgeon’s explanations, confident in their skill, and assured that their surgeon will support them through the entire recovery process.
Additionally, it’s critical to align philosophically—whether a patient prefers a minimalist approach or a more comprehensive, long-term plan. This alignment, much like in a partnership, ensures a collaborative, successful outcome tailored to the patient’s goals and lifestyle.
Ultimately, by prioritizing trust, communication, and shared values, patients can make more informed decisions and achieve better results.
What are the Most Exciting Advances in Minimally Invasive Surgery?
Minimally invasive surgery (MIS) is revolutionizing spine care, offering cutting-edge techniques and technologies that deliver better outcomes with fewer complications and faster recovery times. There is significant progress being made in establishing MIS as a legitimate and effective approach, moving beyond initial skepticism to wide acceptance.
Advances such as robotic and augmented reality technologies are making these procedures more precise and reproducible, ensuring consistent outcomes regardless of the surgeon or location.
Moreover, the evolution of MIS now enables complex procedures to be performed in outpatient settings, reducing hospital stays and costs while improving patient experiences. Beyond the technical innovations, MIS is addressing broader challenges in spine care by alleviating the fear often associated with surgery, helping more patients access the treatment they need. This shift, combined with improved education and patient-centered care, underscores the exciting potential of MIS to transform spine health and restore quality of life.
When Should Patients Consider Minimally Invasive Spine Surgery?
Patients should consider surgery when persistent neck or back pain significantly impacts their quality of life and has not improved after 3-6 months of conservative treatments like physical therapy, injections, or other non-surgical methods.

Prolonged suffering can lead to chronic pain, depression, and reduced effectiveness of even the most advanced surgical techniques. It’s vital to seek a spine specialist early to ensure an accurate diagnosis and appropriate treatment plan.
Fear of surgery often delays necessary care, but minimally invasive techniques now offer faster recoveries and fewer complications. A trusted surgeon will only recommend surgery when absolutely needed and will provide realistic expectations about outcomes.
Addressing symptoms early prevents unnecessary suffering and helps patients regain control of their lives.