What Is ‘Endoscopy’?
The field of spine surgery is rapidly advancing. Traditional surgical techniques utilizing large, open incisions are being supplanted by minimally invasive approaches that allow for less surgical pain, faster recovery, and better overall results. Endoscopic surgeries are one such example of minimally invasive approaches. These approaches are now available for use in spinal surgery, in which a small camera (endoscope) is placed through a tiny incision to remove structures that are pressing on nerves and causing sciatic pain.
For years, orthopedists have been doing shoulder, hip, and knee surgery using arthroscopic cameras. Similarly, general surgeons and OBGYN doctors have used cameras to assist with abdominal surgeries. Frankly, spine surgeons have been slow to utilize this technology, but the delayed adoption hasn’t been for lack of trying! Based on anatomy, scopes are most commonly used to increase visualization in regions that are large enough or that can be expanded. The spine, on the other hand, has much smaller openings and is very sensitive to pressure due to the surrounding delicate nerves.
Endoscopic Microdiscectomy
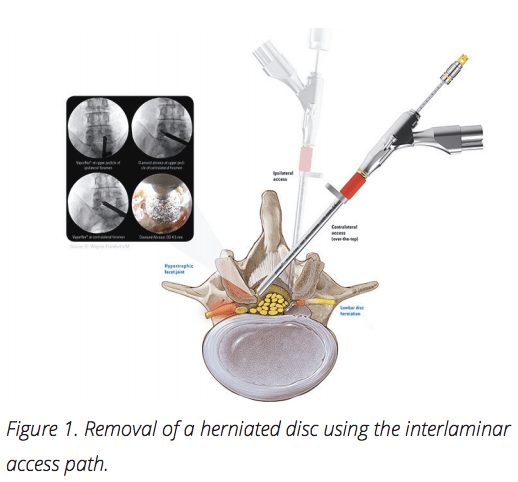
The most common use of endoscopic spine surgery is with lumbar disc herniations. The lumbar intervertebral discs are composed of two major parts: the nucleus pulposus and the annulus fibrosus. The inside ‘jelly’ layer (nucleus pulposus) functions as the shock absorber. The outside layer (annulus fibrosus) is the more structural component that keeps the nucleus contained. When a disc herniation occurs, the nucleus breaks through the annulus, often putting pressure on the nerves and resulting in sciatica. While most disc herniations heal with non-operative treatments, some require surgery. The procedure of choice is often a microdiscectomy in which a small incision is made in the middle of the back, a minimal amount of bone is removed to visualize the disc fragment, and the herniation is removed.
An endoscopic microdiscectomy is technically very different from the conventional microdiscectomy. A smaller incision is made approximately 10cm off to the side of the midline, as opposed to directly over the affected disc. Rather than removing bone to access the herniation, the fragment is removed through an opening called the neuroforamen. The nerves normally exit the spine through the neuroforamen, making it an ideal opening for a small camera (endoscope) to access the discs. Once the disc fragment is visualized, it can then be removed to relieve the pressure of the affected nerve. Furthermore, because of the small incisions, many of these procedures are often able to be performed without general anesthesia, reducing length of stay in hospitals and decreasing overall recovery times.
So why even consider endoscopic surgery when a regular microdiscectomy involves a relatively small incision and works so well? Overall, recovery from both types of microdiscectomy is excellent, with greater than 90% happiness rates reported by patients. However, endoscopy involves an even smaller incision, less muscle disruption, and less bone removal. In essence, it is an enhancement to an already minimally invasive technique. When the two types of microdiscectomy procedures are compared, potential benefits are generally shown in favor of endoscopy with reports of fewer infections, quicker return to work, and less back pain, as documented in scholarly literature.
Other Indications of Endoscopic Spine Surgeries
In addition to disc herniations, research is being done on the use of endoscopic technologies for fusions. Fusions have traditionally required large incisions in order to properly visualize the bony surfaces, a key step that is necessary to get bony growth across a spinal level. However, the small endoscopic camera allows a surgeon to see a magnified image of regions of the spine that may be otherwise difficult to visualize with the naked eye. This opens up the possibility of endoscopic fusions which would revolutionize spinal fusion recovery standards. Implants are actively being designed for these procedures to occur in the near future. Endoscopy also has a role in complex revision lumbar spine surgeries.
Unfortunately, a common cause of revision lumbar surgery is persistent nerve pressure. Because scar tissue is always created after the first surgery, there is an increased risk of spinal fluid leak where the scar tissue becomes adherent to the nerves. An endoscopic surgery uses a different surgical approach through undisrupted tissue planes, reducing the amount of internal scarring that is encountered. While beneficial in many applications, not every surgery should be done endoscopically. Although disc herniations are the current best indication for endoscopy, there are many circumstances where the nerves are being pinched by both the disc and overgrown bone.
A more conventional microdiscetomy would usually be preferred in such cases because the technique allows for easier bone resection. If there is major instability, a fracture, or scoliosis, endoscopy alone isn’t as successful as other surgical techniques either. Lastly, endoscopy is not commonly used in the cervical spine; although patients with pinched nerves in the neck are not currently candidates for this technology, perhaps they will be in the future.
The Future of Endoscopy
While there are limitations, the future of endoscopy within spinal health is bright. Current spinal applications are very successful and the scope of this ultra-minimally invasive technology is rapidly growing.
Read more in our Journal.

by Dr. Colin Haines, M.D., Virginia Spine Institute