By Dylan C. Dean, MD, USC Spine Center
Jeffrey C. Wang, MD, USC Spine Center
What is Cervical Radiculopathy?
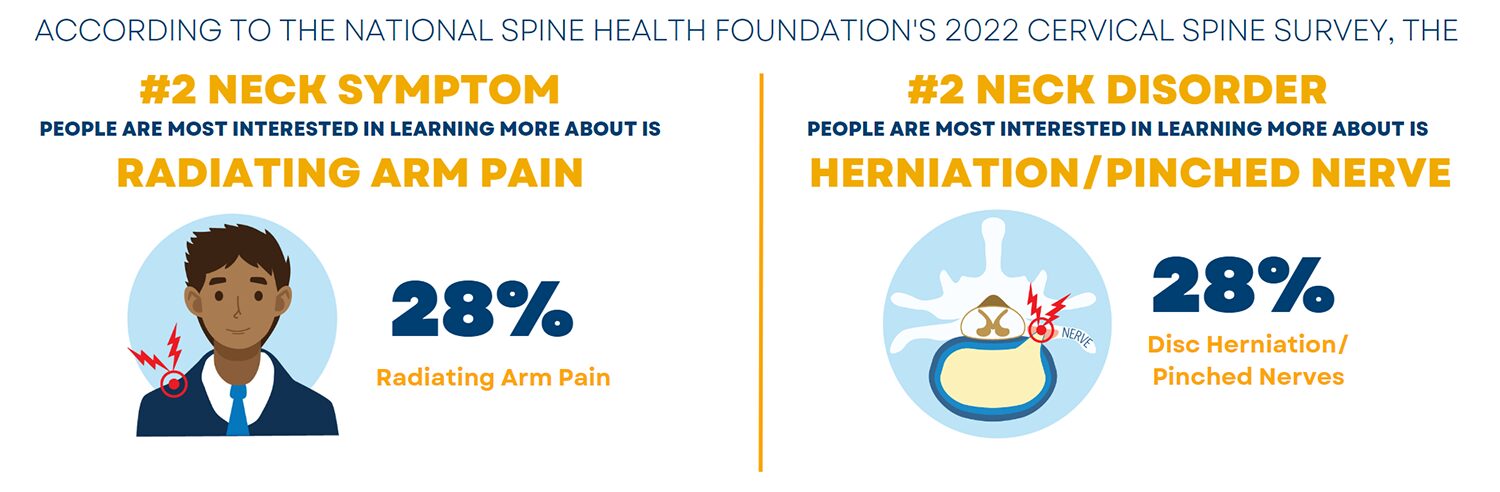
Cervical radiculopathy occurs when a nerve root in the neck becomes pinched by something pressing on it, such as a herniated disc or arthritic bone spur. This can cause numbness, weakness, and pain that radiates from the neck to the shoulder or arms. Because these episodes usually resolve with time, surgery is reserved for refractory cases or for those with progressive symptoms. When conservative management fails, there are several highly successful surgeries that decompress the affected nerve root.
What are the Causes?
Nerves in the neck can become compressed or irritated in several different ways to cause cervical radiculopathy. In a disc herniation, the rubbery disc material protrudes out from between the cervical vertebrae and irritates the nerve. In degenerative arthritis, one of these cushioning discs can develop excessive wear, which leads to excessive motion and bone spurs that impinge upon the nerves. Other sources of compression include changes related to injury, tumors, and cysts.
What are the Symptoms?
There are many different cervical pathologies that can become symptomatic, often with overlapping features. Cervical radiculopathy typically presents with pain, weakness, or changes in sensation down the arm(s). This differs from axial neck pain, where the pain is localized to the neck, and from cervical myelopathy, where the spinal cord itself is compressed causing imbalance and poor coordination. Symptoms, clinical features, neuroimaging, and electrodiagnostic testing help differentiate cervical radiculopathy from these other pathologies and help pinpoint the exact nerve root(s) affected.
Making the Diagnosis
X-rays are usually the imaging study obtained initially and are helpful in demonstrating degenerative changes, including bone spurs and decreased cervical disc height. Special flexion (forward bending) and extension (backward bending) x-rays can reveal instability as the patient bends their neck looking for movement between vertebrae as a source of compression. MRI scans show the soft tissues, including herniated discs, cysts, tumors, and the nerve roots themselves and whether they are compressed. CT scans can highlight areas of bony compression with detail and are often obtained for preoperative planning.
Electrodiagnostic studies include nerve conduction studies (NCS) and needle electromyography (EMG) which measure the electrical activity of the nerves and muscles. They can help differentiate radiculopathy from other conditions such as carpal tunnel syndrome and diabetic neuropathy. In addition, they highlight which nerve roots are affected, and are therefore especially useful when patient symptoms and imaging alone do not pinpoint which nerves to decompress.
Non-operative Treatments
Non-operative treatment is successful in most patients, therefore surgical decompression is reserved for those with progressive deficits or who have failed conservative management. There are several non-surgical treatments available, but whether they improve recovery or simply provide symptomatic relief is unclear. Treatments include physical therapy, immobilization with a cervical collar, traction, medications, oral corticosteroids, and steroid injections. Selective nerve root blocks are helpful both diagnostically and therapeutically, as they can be injected around a single nerve root of interest. Thus, if effective, these injections can confirm the source of radiculopathy in cases of multilevel disease.
Surgical Options
Cervical disc arthroplasty (CDA) places an artificial disc into a decompressed disc space and is one of the preferred treatments due to its ability to preserve neck motion. It is often used in cases of single or two-level disease and should be avoided in those with symptomatic neck joint arthritis, as the preserved motion can worsen pain. In cases of cervical radiculopathy with significant arthritis or instability, fusion may be the better choice. In these surgeries, several vertebrae are fused with bone graft or implants to provide stability, which is especially important when large segments of bone must be removed for neural decompression. Anterior cervical discectomy and fusion (ACDF) remains the gold standard surgery with a high success rate. Advantages include low infection rates and wound complications. Potential disadvantages include failed fusion (pseudoarthrosis) as well as problems with speech and swallowing, which can happen with any anterior exposure. Posterior foraminotomy is another alternative to a fusion and has the major advantage of being done minimally invasively. It avoids the potential complications associated with entering through the front of the neck and may be preferred in those whose anatomy makes an anterior neck exposure contraindicated. Not everyone is a candidate however, and it should generally be avoided in patients with large central disc herniations or instability.
Conclusion
Cervical radiculopathy can be caused by several issues in the neck and can be treated both non-operatively and operatively. If symptoms of radiating arm pain, weakness, or numbness do not resolve quickly, seeking the opinion of a spine health specialist is warranted to guide the proper treatment.