With increasing life expectancy, a growing number of men are now affected by osteoporosis—a condition historically perceived as predominantly affecting women. This article examines the causes, clinical manifestations, and treatment options for osteoporosis and low bone density in the male population
What is Osteoporosis?
Osteoporosis is a bone disease that appears when bone mineral density decreases—causing the affected bones to become more fragile and prone to breaking.
The Scope of the Issue
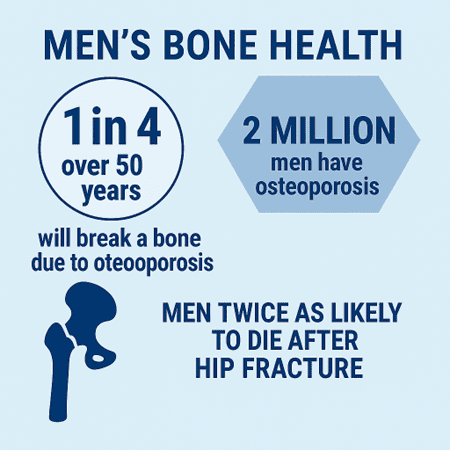
The dangers of osteoporosis and low bone density are real. Studies have shown that the incidence of osteoporosis-related fracture in men is similar to that of myocardial infarction and exceeds that of lung and prostate cancer combined. In fact, about 1 in 4 men over the age of 50 will break a bone due to osteoporosis. Not only that, up to 2 million American men have osteoporosis, with an additional 12 million American men at risk.
Furthermore, studies have shown that men with osteoporosis and low bone density are twice as likely to die after a hip fracture compared to women with osteoporosis.
One factor contributing to the high rates of injury and mortality among men is the delayed diagnosis and limited screening for conditions like osteoporosis. As highlighted in the article, men receive significantly less screening and treatment compared to women. With life expectancy on the rise, the number of men affected by osteoporosis and low bone density is expected to grow—making regular checkups essential for maintaining overall health.
Types of Osteoporosis
Different types of osteoporosis affect the body similarly.
- Primary Osteoporosis:
- Type 1 (postmenopausal osteoporosis): Occurs in women after menopause due to estrogen deficiency, often starting around age 50 years.
- Type 2 (senile osteoporosis): Occurs due to age-related reduction in calcium absorption, vitamin D deficiency, and impaired bone formation in both men and women over the age of 70 years. Men with osteoporosis most commonly suffer from the senile type.
- Secondary Osteoporosis: Occurs due to medications, lifestyle factors, and medical conditions that affect bone metabolism. The list of offenders is extensive, but here are a common few:
- Smoking
- Sedentary lifestyle
- Malnutrition
- Alcohol abuse
- Long-term oral steroid use
- Some medications for acid reflux
- Some cancer treatments
- Endocrine disorders (diabetes and hormone disrupting conditions such age-related testosterone decline in men)
Biological and Hormonal Factors
On average, men tend to have greater bone mass than women, leading to osteoporosis impacting them later in life. As such, men experience a loss of bone mass at a slower rate, typically starting in their 60s.
Bone density is greatly influenced by hormones such as estrogen and testosterone. Both estrogen and testosterone help regulate the process of bone remodeling — a process that helps break down old bones and creates new, healthy bones. While estrogen is a key factor in preventing bone loss, both estrogen and testosterone help maintain bone formation.
Similarities and Differences for Men and Women
Similarities in Bone Health Between Men and Women
| Aspect | Details |
| Bone physiology | Both sexes experience continuous bone remodeling involving osteoclast (resorption) and osteoblast (formation) activity. |
| Peak bone mass | Achieved in early adulthood (typically by age 30) in both men and women. |
| Aging-related bone loss | Bone density decreases with age in both sexes, especially after age 50. |
| Fracture risk increases with age | Risk of fractures (especially hip, spine, and wrist) rises with age for everyone. |
| Impact of lifestyle factors | Poor diet, smoking, excessive alcohol, and inactivity negatively affect bone health in both. |
| Role of calcium and vitamin D | Both men and women require adequate intake for optimal bone maintenance and remodeling. |
| Importance of weight-bearing exercise | Weight-bearing and resistance exercises improve or maintain bone density for both sexes. |
| Diagnostic tools | Bone Mineral Density (BMD) tests (e.g., DXA scans) are used to assess osteoporosis in both. |
| Pharmacologic treatment options | Medications like bisphosphonates, denosumab, and teriparatide are effective in both sexes. |
| Fall prevention benefits | Minimizing fall risks through balance training and home safety reduces fracture risk equally. |
| Hormonal influence | Hormones (estrogen in women, testosterone in men) regulate bone turnover in both sexes. |
| Bones | Conditions like corticosteroid use, chronic disease, and malabsorption affect bone similarly |
Differences in Bone Health Between Men and Women
| Aspect | Men | Women |
| Hormonal changes | Gradual decline in testosterone with age | Sudden drop in estrogen after menopause |
| Most common type of osteoporosis | Type II (senile) | Type I (postmenopausal) |
| Age of onset | Typically begins later (after age 70) | Often begins earlier (postmenopause, around age 50) |
| Fracture patterns | More prone to hip and vertebral fractures | More prone to vertebral, wrist, and hip fractures |
| Secondary osteoporosis | More common (due to medications, comorbidities, hypogonadism) | Less common, but still significant |
| Diagnosis rates | Underdiagnosed and undertreated | More likely to be screened and treated, especially postmenopause |
| Bone loss rate | Slower and more gradual bone loss | Faster and more pronounced, especially after menopause |
| Mortality after hip fracture | Higher in men | Lower, though morbidity remains high |
| Screening guidelines | Often overlooked unless risk factors are present | Routine DXA screening recommended postmenopause |
| Public perception | Still seen as less susceptible to osteoporosis | Widely recognized as at higher risk, leading to better awareness |
How to Get Diagnosed
Because men are screened for osteoporosis less frequently, diagnosis often occurs at a later stage—typically following a fracture. Even after diagnosis, men are less likely to pursue treatments, influenced by a combination of social norms and behavioral factors.
Further highlighting the problem, The United States Preventive Services Task Force (USPSTF) creates recommendations on preventative services like screening tools. In the absence of available data regarding men and osteoporosis, they lack specific screening guidelines for men, which is in great contrast to the well-established recommendations it has for osteoporosis in postmenopausal women.
If you are at risk for osteoporosis (all men aged 70 years or older plus younger men with other risk factors), it is recommended to get a DEXA scan to determine if the bones are healthy and check for osteoporosis and low bone density.
Even at home there are ways to see if you or someone you know may be at risk. For example, it is possible to use online tools such as FRAX to evaluate the risk of a fracture. It is extremely important for men to discuss their FRAX results with their healthcare professional.
Treatments for Osteoporosis
If you are diagnosed with osteoporosis or low bone density, there are many ways to improve bone health:
A change in lifestyle:
- Nutrition: Adequate calcium (1,000–1,200 mg/day) and vitamin D (800–1,000 IU/day).
- Weight-bearing and muscle-strengthening exercises.
- Smoking cessation and limiting alcohol intake.
Pharmacologic treatments for osteoporosis in men:
| Class | Medication (Brand) | FDA-Approved | Key Benefit |
| Bisphosphonates | Alendronate (Fosamax), Risedronate (Actonel), Zoledronic acid (Reclast) | ✅ Yes | ↑ BMD, ↓ fracture risk |
| Anabolic Agents | Teriparatide (Forteo), Abaloparatide (Tymlos) | ✅ Yes | ↑ Bone formation, ↓ Fractures |
| RANKL Inhibitor | Denosumab (Prolia) | ✅ Yes | ↓ Bone loss, ↑ BMD |
| Hormone Therapy | Testosterone (various forms) | ⚠️ Hypogonadism only | ↑ BMD, limited fracture data |
| Sclerostin Inhibitor | Romosozumab (Evenity) | ❌ Not yet | Promising, not yet approved |
Monitoring and Follow-Up
It is recommended to get bone density testing every 1-2 years depending on initial results and other factors, including an increase in risk factors. Additionally, regularly check for any negative reactions from treatments while staying consistent with the prescribed treatment plan.
The Need for Awareness and Advocacy
As diagnoses of osteoporosis and low bone density increase among men, it becomes increasingly important to challenge the stigma around men seeking medical care and routine checkups. Without addressing this issue, more men will continue to experience the serious and long-term consequences of osteoporosis-related fractures. Regular screenings are essential for early detection and prevention, helping to reduce the risk of these avoidable injuries.
Conclusion
Osteoporosis and low bone density are a common but serious part of aging. Millions of men go undiagnosed until a life-changing fracture occurs. It is necessary to realize the importance of bone health in men and normalize regular checkups. Use this information to become your own best advocate for men’s bone health and discuss a baseline screening with your healthcare provider.



