Bone Proteins in the Neck
Introduction
The Spinal Research Foundation investigated the use of BMP to promote bone fusion in the vertebrae of the neck. Although previous BMP studies have found increased risk of complications associated with the use of BMP in cervical fusions, SRF’s clinical study found only a small percentage (2.9%) of patients experienced complications related to the use of BMP. Additionally, when used in small doses, BMP used in cervical fusions led to strong improvements in disability, pain, and general health. This shows that limited use of BMP in spinal fusions in the neck can promote good outcomes by promoting high fusion rates with very few complications.
Research Summary
- When used in small doses, BMP used in cervical fusions led to strong improvements in disability, pain, and general health
- Only a small percentage (2.9%) of patients experienced complications related to the use of BMP
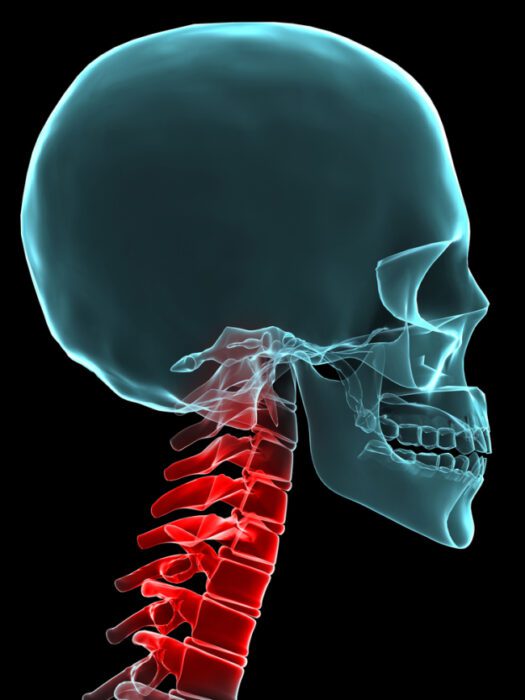
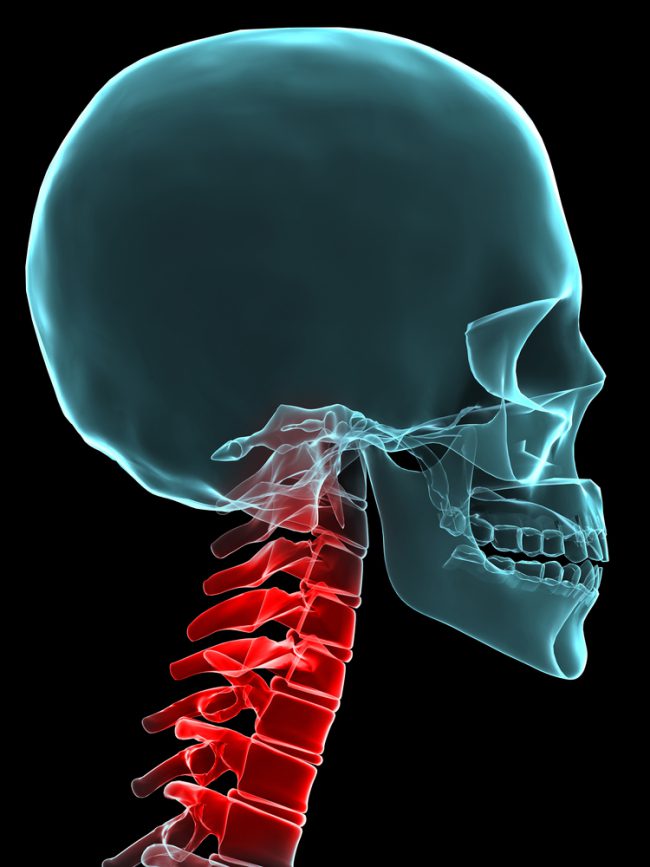
Back and neck pain can occur from stress on spinal discs. This stress can cause damage to the discs. A type of treatment for degenerated discs is a fusion surgery. Spinal fusions involve a surgeon removing the damaged disc(s) and promotes bone fusion between the vertebrae using a bone graft. Often times, the surgeon will harvest bone tissue from the patient’s hip (called an autologous graft) and use this ground bone to promote fusion in the spine. Implant cages are put in to maintain disc space while the bone is growing. The harvesting of the bone graft requires an additional surgery and can potentially cause lingering pain at the graft site.
BMP is an alternative to the use of autologous bone grafts to promote bone formation and growth. BMP has been approved for vertebrae fusion in the lower back (lumbar spine), but the use of BMP spinal fusion in the neck (cervical spine) has varied results. There were reports of life-threatening side effects associated with the use of BMP in the neck, so the FDA issued a warning about the complications that could occur in the cervical spine.
Only a few patients in our study have had complications with small doses of BMP. In fact, 1-year and 2- year post surgery results were significantly improved over the pre-surgery. Neck and arm pain were much improved after the surgery. Neck disability was also greatly improved. 98% of the patients achieved a successful fusion. Even in surgeries that were at a greater risk of non-union (unsuccessful fusion).
Previous studies show a greater rate of complications with BMP use in neck fusions. Only 24 (10% of the patients) of the patients in SRF’s study had complications that required medical attention. Out of which, only 7 patients (or 3% of the total patients) had issues related to the use of BMP in their neck fusion.
In our study BMP use for neck fusions results in improved patient outcomes. There is a low rate of complications. In addition, use of BMP led to high rates of successful fusions. These findings suggest that BMP might be a viable treatment option for certain spinal patients.