What is adolescent scoliosis?
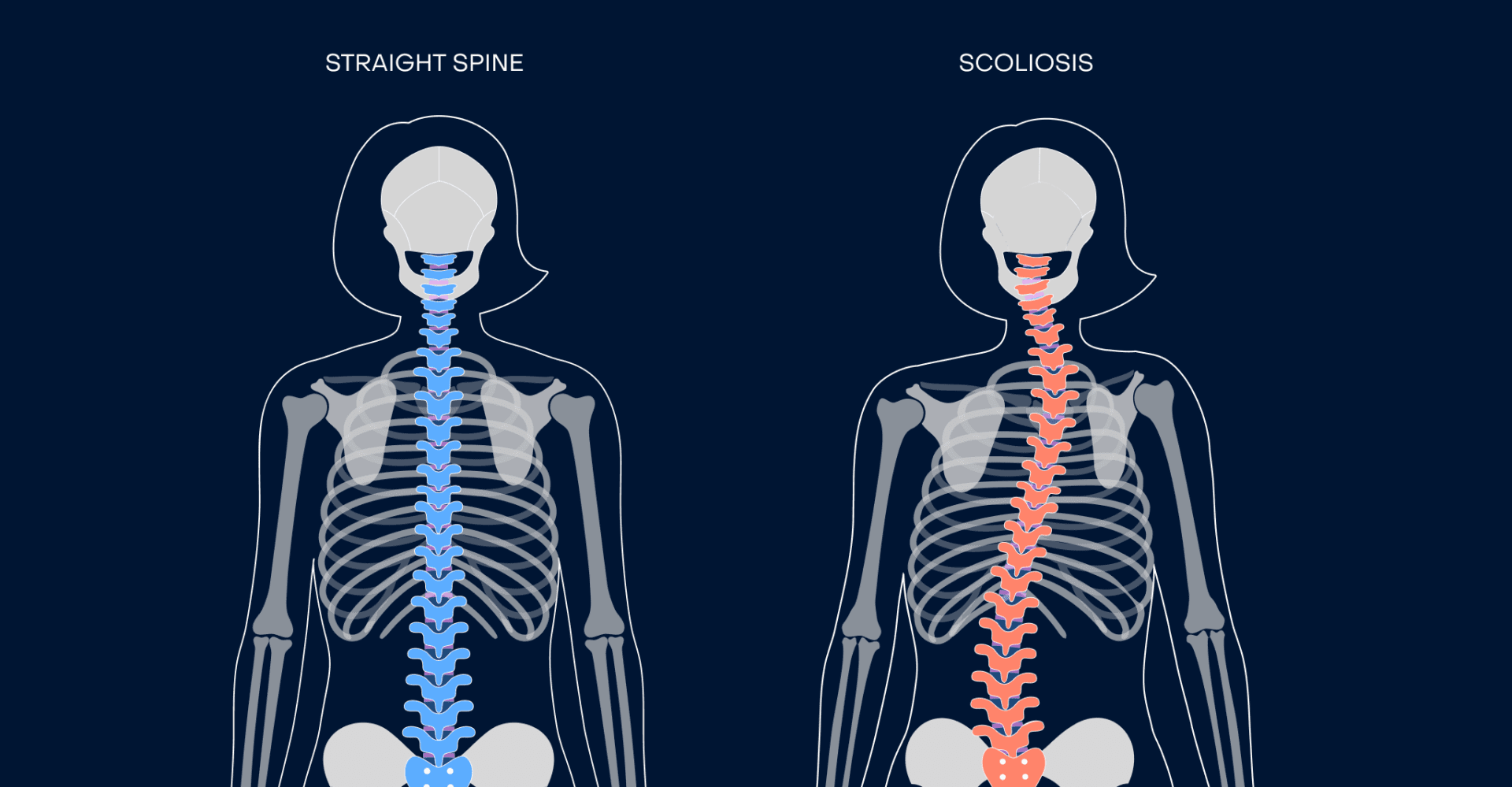
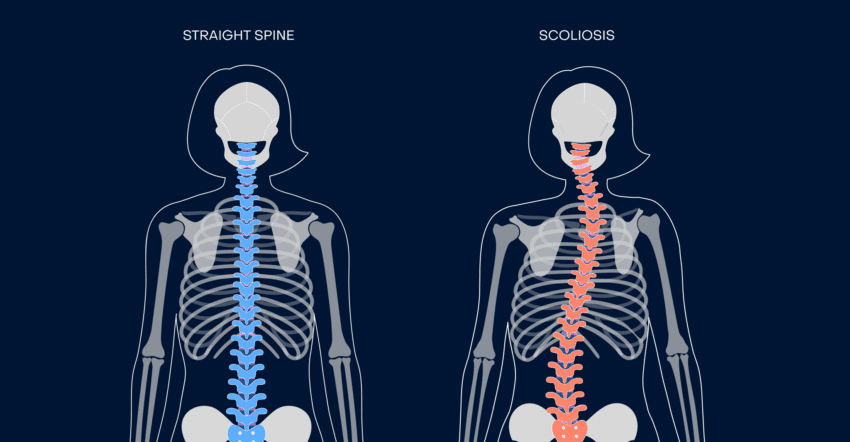
Scoliosis is an abnormal curvature of the spine in the front-to-back plane or view of the body. It affects millions of people worldwide, posing unique challenges that require attention and support. In people with scoliosis, the spine can curve to the left, right, or both.
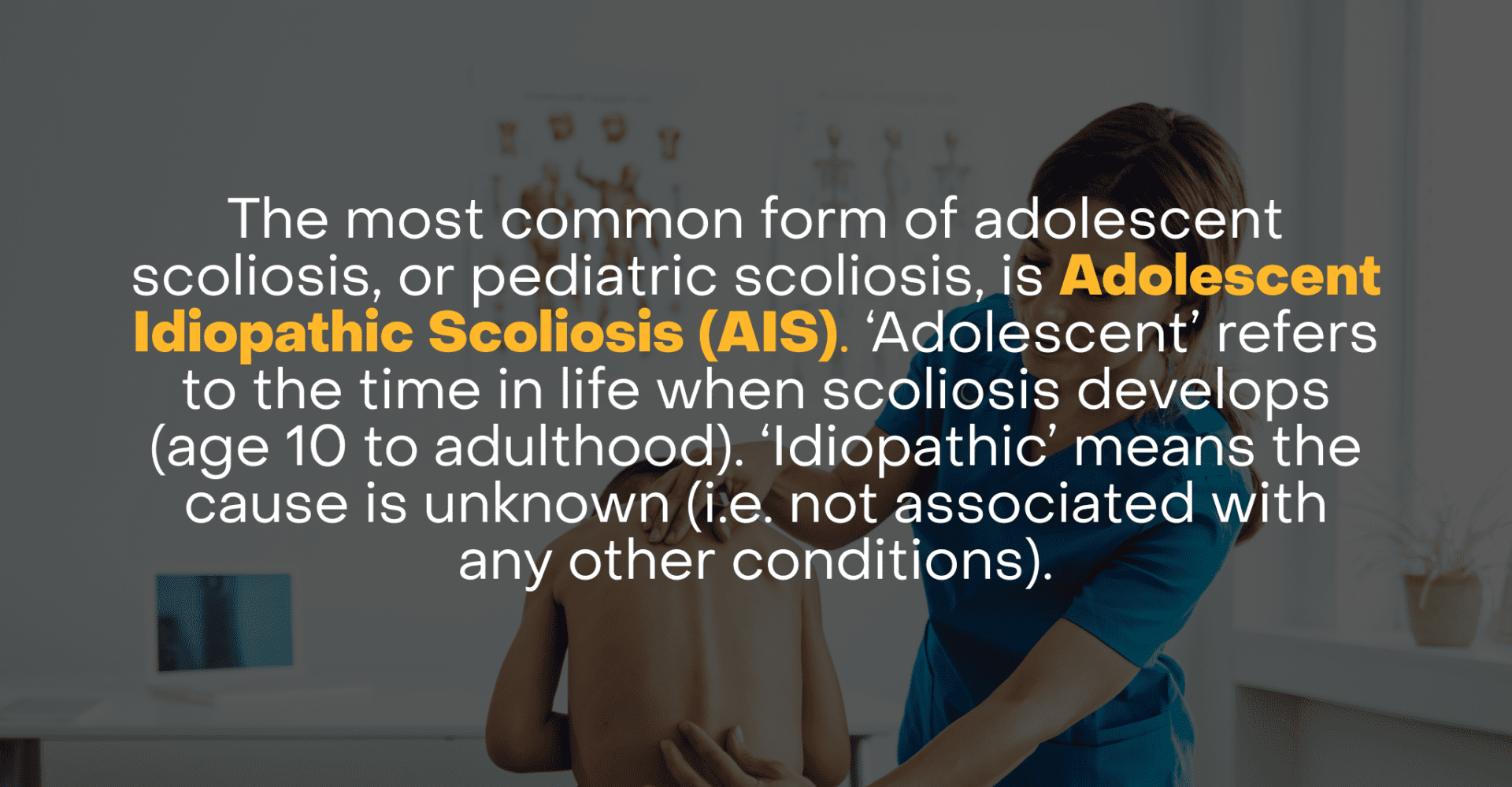
There are three types of pediatric scoliosis (also known as childhood scoliosis and adolescent scoliosis): Congenital Scoliosis, Neuromuscular Scoliosis, and Adolescent Idiopathic Scoliosis (AIS).
Congenital Scoliosis is caused by a malformation of the spine during fetal development. Vertebrae may be improperly formed or fused together, leading to a curvature of the spine that is present at birth. The condition can worsen as the child grows. This is the least common type of pediatric scoliosis.
Neuromuscular Scoliosis is associated with neurological or muscular conditions like cerebral palsy, muscular dystrophy, or spinal cord injury. The muscle imbalances in the muscles supporting the spine lead to the development of scoliosis.
Adolescent Idiopathic Scoliosis (AIS) is the most common form (approximately 80%) of pediatric scoliosis, and is the focus of this article. ‘Adolescent’ refers to the time in life when scoliosis develops (age 10 to adulthood). ‘Idiopathic’ means the cause is unknown (i.e. not associated with any other conditions).
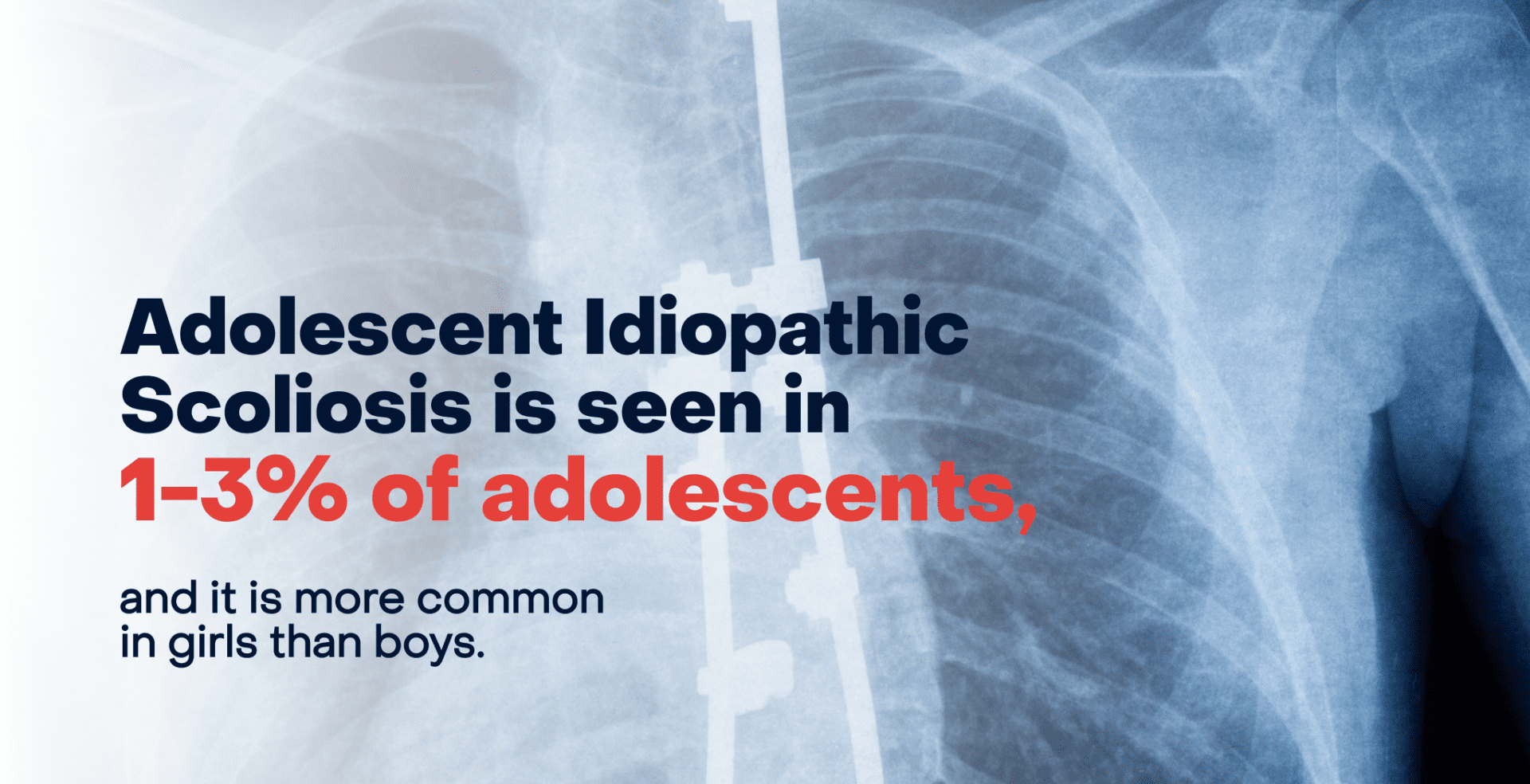
AIS is seen in 1-3% of adolescents, and it is more common in girls than boys. Girls also tend to have progressive cases of scoliosis compared to boys. These gender differences are not totally understood, but have been linked to rapid growth patterns, hormones, and inheritance patterns. However, the condition is usually mild for most adolescents.
In adolescents, the most common idiopathic curve pattern is a right thoracic curve (see our Spine Glossary for more detail on the parts of the spine and common terms). If a left thoracic curve is diagnosed, then further testing is warranted looking for a non-idiopathic reason for the curvature.
What causes Adolescent Idiopathic Scoliosis?
The cause(s) of AIS is not fully understood, but genetic, metabolic, hormonal, and biomechanical factors have been thought to be contributing factors.
What we do know is that AIS has a large genetic component, which means that there are no medical or nutritional interventions that can prevent this component. If a family member has scoliosis, the likelihood of developing it increases. Researchers have identified certain genes that may contribute to its development, but the genetic link is complex, likely multifaceted, and not fully understood.
There is some evidence to suggest that uneven growth rates between the front and back portion of the vertebrae may be one contributing factor of the development of AIS.
Contrary to some beliefs, wearing heavy backpacks or not drinking enough milk does not cause scoliosis in adolescents.
Because the cause(s) of AIS is not known, a doctor’s focus is typically on monitoring for early detection and on appropriate treatment strategies.
What are the signs and symptoms of Adolescent Idiopathic Scoliosis?
The spinal column should be straight when viewed from the front or back. In adolescents with AIS, the spine is curved to the left, right, or both. This type of scoliosis often becomes noticeable during the peak growth spurts of adolescence. Most children and teens with mild scoliosis do not have symptoms or pain.
In adolescents with AIS, you might see that one shoulder or hip is higher than the other, or one shoulder blade is more prominent. Clothes may not hang straight, or there may be an unequal distance between the arms and body when standing.
It is common for parents not to notice any signs at all – and this is okay! Sometimes AIS is not noticed or even visible until an exam at the child’s routine checkup. AIS is most noticeable when bending forward, which is part of the physical examination for AIS screening.
How is Adolescent Idiopathic Scoliosis diagnosed?
AIS causes the spine and ribcage to rotate (twist) as the spine curves. This rotation is what doctors check for in an examination. Typically, the rotation is visible when a patient bends forward (this is known as the Adams forward bend test). While bending, the clinician may use a level, known as a scoliometer, to estimate the degree of asymmetry. Scoliosis is also typically confirmed with a diagnostic standing X-ray. Laying X-rays should be avoided because the body (and spinal curves) tend to relax in the lying position, giving an inaccurate assessment of the spine.
The curve of the spine is measured in degrees, as an angle, called a Cobb angle. Scoliosis is defined as a curve greater than 10 degrees but the severity can vary depending on the angle.
- Mild Curve: A curve of 20 degrees or less.
- Moderate Curve: A curve of between 25-40 degrees.
- Severe Curve: A curve of more than 50 degrees.
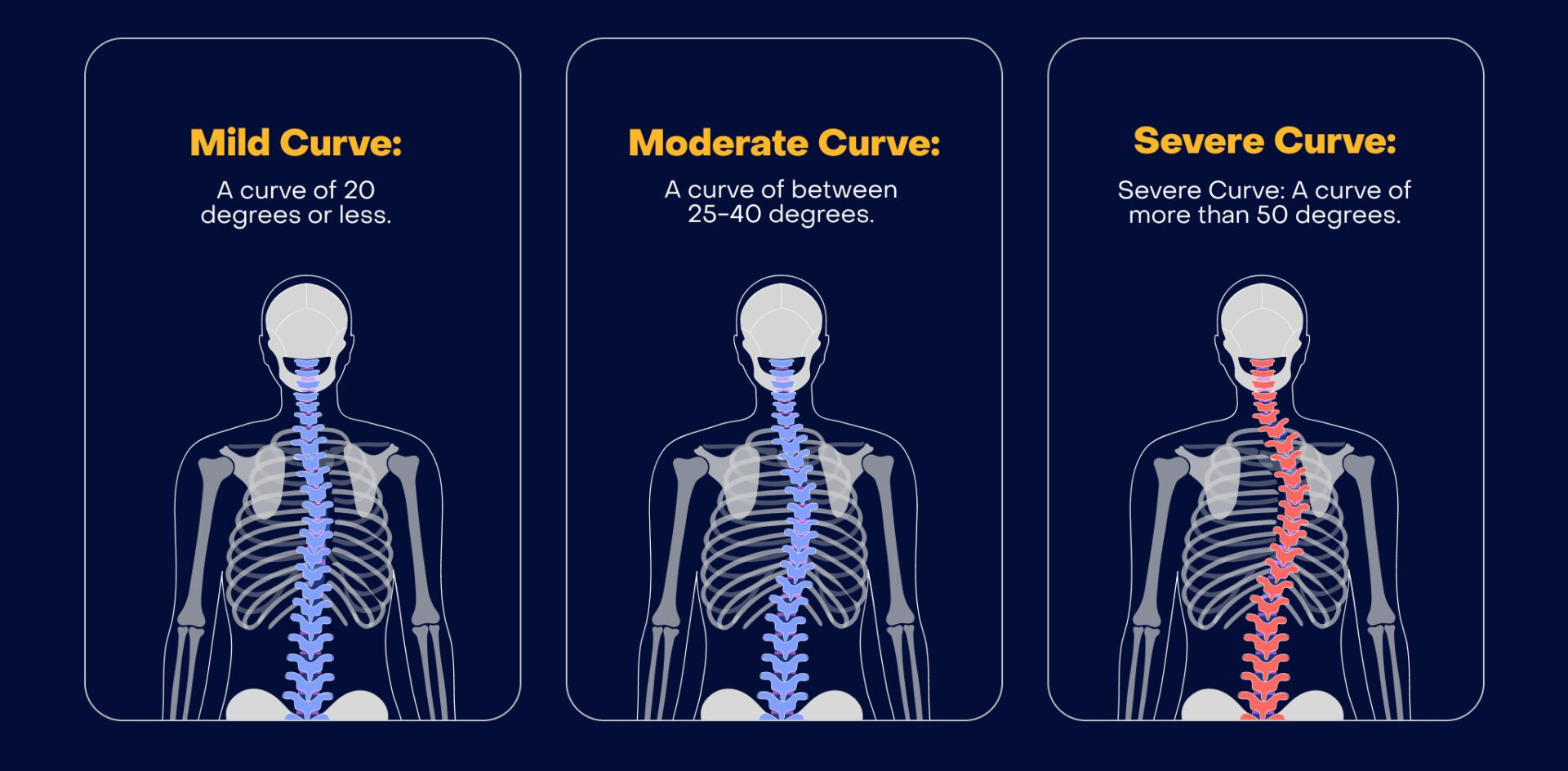
Approximately 10% of the population has small curves (less than ten degrees), which don’t affect function or health. This condition is called Spinal Asymmetry.
Does scoliosis cause back pain in adolescents?
The relationship between back pain and adolescent scoliosis is inconclusive, and AIS was long considered to be painless. Some more recent studies indicate that there is more frequent, significant, and longer duration of back pain in adolescents with idiopathic scoliosis than in similar control groups without scoliosis. However, another study found back pain to occur in some adolescents with scoliosis, but did not find this to be problematic in the majority of AIS patients.
In many cases, adolescents with scoliosis who do experience pain could have coexisting conditions, and low back pain becomes increasingly prevalent with age among all adolescents irrespective of scoliosis. Research shows that 30% of all adolescent girls and 26% of adolescent boys experience lower back pain, and 11% of all adolescents experience chronic back pain that lasts longer than 3 months. This pain could be caused by lifestyle factors, growth patterns, hormones, obesity, spinal issues, or other factors.
How is Adolescent Idiopathic Scoliosis treated?
There are three main treatment options for adolescents with scoliosis: to monitor it with routine check-ups which may include x-rays, to wear a brace, or to have surgery. Surgery is the only way to permanently change the curve of the spine while preventing it from getting worse.
Most adolescents with AIS do not have curves that progress to the degree where surgery is recommended, yet AIS is the most common reason for elective orthopedic pediatric surgery. The greatest risk of progression occurs during periods of rapid growth, most commonly during the adolescent growth spurt.
In general, the younger the patient and the larger the curve(s) at the time scoliosis is identified, the greater the potential for progression. Treatment plans will depend on the patient’s age and the degree of curvature.
If a teen has finished growing, and the curve has progressed but is less than 40 degrees, there is little risk that the curve will progress rapidly in adulthood. During adulthood, curves tend to increase by about one degree each year, which is a factor when considering various treatments.
Ultimately, choosing between operative versus nonoperative interventions comes down to a detailed discussion of risks and benefits of each option between the patient, the parents, and their doctor.
The risks of each treatment option must be weighed against the likelihood and degree with which the quality of life is expected to improve with each treatment. It is also important to recognize that a nonoperative treatment plan may change over time for patients.
1. Monitoring with routine check-ups
If the scoliosis is mild and not causing any functional problems, regular monitoring by a doctor is often the first step, which may include periodic X-rays. This allows the clinician to monitor the curve size as the adolescent grows, looking for worsening that might change the treatment plan.
Observation is usually recommended for patients who are still growing with curves that measure less than 20 to 25 degrees and for patients who have finished growing with curves that measure 40 to 45 degrees.
Alternatives to traditional X-rays are now available at some centers. Ultra low dose imaging with special slot scanners can obtain very high quality images of the spine and lower extremities at a lower dose of radiation.
2. Wearing a brace
If the curve is more pronounced or progresses during growth spurts, bracing might be recommended. Orthopedic doctors typically recommend scoliosis bracing for teens who are still growing and have a curvature of about 25 degrees or more. Bracing is not recommended for patients with AIS who have reached skeletal maturity.
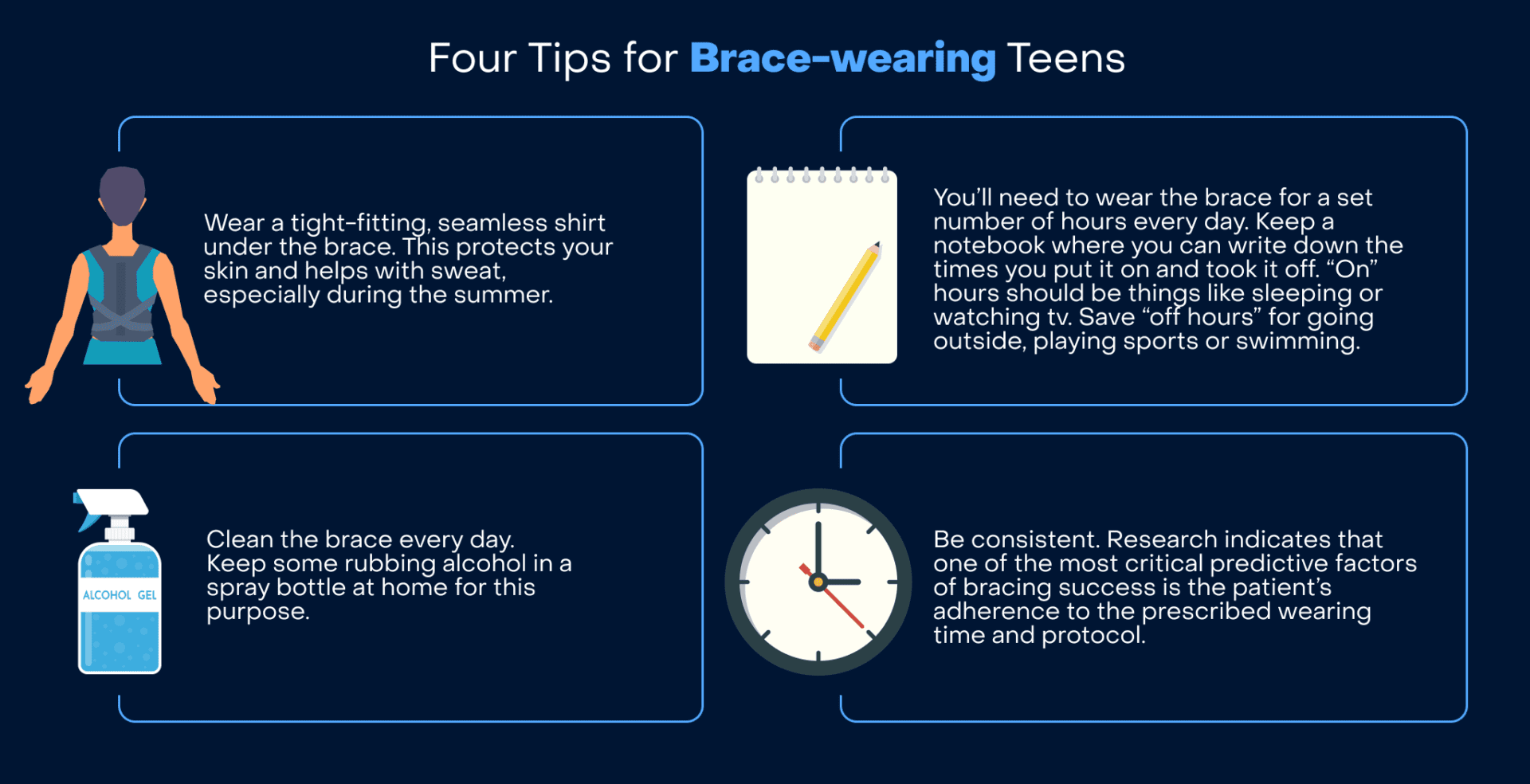
It is important to know that braces don’t cure scoliosis or reverse the curve. The purpose of a brace is to help prevent further worsening of the curvature during the adolescent’s growth period. A successful course of bracing prevents the need for surgery.
The brace is fitted specifically to the patient’s spine. The brace must be worn daily for the hours prescribed by the doctor to be effective. Generally, adolescents with moderate scoliosis wear their brace between 12 and 20 hours a day. Sports should continue even if a brace is recommended, and is often taken off during these times.
Standing X-rays taken with the brace on are helpful to assess that the brace is putting pressure on the right locations of the curvature. If the brace is correctly fitted, X-rays taken in the brace will make the curve appear smaller. To assess if the curve is progressing during brace treatment, Standing X-rays must be taken at least several hours after the brace has been taken off, to get an accurate image of the spinal curve.
Depending on how long before skeletal maturity is reached, bracing treatment may be several years. It’s important to note that once a brace is removed after years of regular use, a weakening of the core may be noticeable by the teen. Physical therapy can help alleviate this through core strengthening.
Did you know? An orthotist is a professional who specializes in fitting and making braces.
3. Surgery for adolescents with AIS
In cases where the curve is severe (typically over 40-50 degrees), or if it continues to worsen rapidly, surgical interventions might be recommended. If left untreated and allowed to progress further, more severe curves are associated with reduced lung volumes, pain, and physical dysfunction.
The most common surgical corrective procedure is spinal fusion, where the curved vertebrae are fused together so they heal into a single, solid bone. This is intended to prevent further curvature and stabilize the spine.
In spinal fusion surgery, rods and screws are attached to the vertebrae at the section of the spine that is affected by the curvature. Surgery is most commonly done through an incision on the back. Patients are typically in the hospital for several days, and should expect to miss three to four weeks of school. At six to twelve weeks after surgery, most adolescents are back to most of their normal activities except for high impact activity/sports restrictions that may continue depending on their surgeon’s recommendations.
Many parents assume they should wait until their teen is done growing to have surgery, but the timing of surgery is multifactorial and individualized depending on each patient’s growth, progression, and curve pattern. Waiting until adulthood is not typically recommended because it is easier to correct the smaller, more flexible curves in a child or teen’s spine than an adult’s, and this can mean a less complicated surgery, and the potential that fewer vertebrae need to be fused.
Two alternatives to spinal fusion for adolescent idiopathic scoliosis
In the past few years, significant advancements have been made in spinal fusion to treat scoliosis. This includes two alternatives to spinal fusion for adolescents with idiopathic scoliosis.
1. Vertebral Body Tethering (VBT)
This is a technique gaining in popularity which offers a smaller subset of qualifying patients an alternative to spinal fusion, and the results appear promising. This technique uses anchors and a flexible cord to guide the spine into an upright alignment.
Generally, patients need to be between the ages of 8 and 16, have spinal curves greater than 35 degrees and less than 65 degrees, have a specific curve pattern, and have significant spinal growth left. As of 2024, VBT is only conditionally approved in the U.S. for patients who have failed or are not candidates for brace treatment.
2. ApiFix
A posterior but fusionless surgery developed by ApiFix recently received conditional approval from the FDA in the United States for use in adolescent idiopathic scoliosis.
This system involves a self-adjusting rod that acts as an internal brace to help straighten the spine over time. The rod allows a greater degree of motion compared to fusion surgery. It is considered less invasive than fusion, and patients are typically discharged from the hospital in 1-2 days and return to school within 2 weeks.
This new technique shows promising early results, but lacks long-term data thus far.
Do alternative treatments help with AIS?
There are some claims that alternative treatments can help prevent scoliosis from worsening, including acupuncture and acupressure, electrical stimulation, physical therapy, nutritional and vitamin supplements, and chiropractic manipulation. But there is no medical or scientific data that proves alternative methods will affect the progression of scoliosis.
Instead, treatments like traditional physical therapy are designed to help a teen maintain an active lifestyle. One key element of physical therapy is core strengthening. This is especially important for teens who wear a brace, because it can help keep their back strong so that their condition does not deteriorate when they stop wearing the brace.
The key to success in physical therapy is making sure you continue stretching and strength building exercises at home. These should become a part of your daily routine to achieve sustainable benefit beyond the duration of the physical therapy program.
However, there is early research in Physiotherapy Scoliosis Specific Exercise (PSSE), like the Schroth Method. These are exercises that specifically address posture, spinal balance, and core strength in patients with scoliosis. These exercises may play a role in slowing down progression in mild or moderate curves.

For more information, we recommend visiting Setting Scoliosis Straight, a non-profit organization devoted to empowering families impacted by scoliosis through education, connection, and research.
Summary: What Parents Should Know
- Adolescent Idiopathic Scoliosis has a strong genetic component and isn’t caused by anything you or your child did or didn’t do.
- AIS often becomes noticeable during the peak growth spurts of adolescence.
- Treatment depends on the degree and progression of the spinal curve.
- Kids and teens with AIS can and should keep playing sports and pursuing healthy activities.
- If your adolescent needs surgery, they may have an easier recovery if the surgery occurs while the curve remains flexible.
- No matter what treatment is utilized for AIS, it is important for adolescents to understand that they need to prioritize their spinal health throughout their lives, including maintaining a healthy weight, staying active, keeping a strong core, and never becoming a nicotine user.
- Have hope: Adolescents with scoliosis can live active, healthy lives!