I am an active seasoned citizen (72 years old) who retired from the military and then taught high school math for 15 years at South Lakes High School and McLean High School. I am now fully retired, and part of my routine includes a workout in the gym once a week by warming up on a treadmill for 10 minutes, lifting an accumulation of 20,000 pounds, then riding a stationary bike for 25 minutes. Additionally, I play tennis and/or golf once a week, and occasionally I volunteer with both Habitat for Humanity and Food for Others. All of my activities require some strength and flexibility.
Around 2011, I started to have occasional numbness in my right arm and thumb. This was an annoyance, but the numbness was temporary and I could still do almost everything. I also had strange neck cramps for no apparent reason. Then at the beginning 2014, my whole right arm hurt and became numb whenever I looked up. This progressed with the pain and numbness occurring frequently just looking straight ahead.
Luckily, I could relieve my symptoms by putting my chin to my chest for a few seconds. It was almost comical to watch me lowering my head at strange times to alleviate the pain, but less comical when I was driving a car. I did a lot of research, consulting many sources to determine the very best doctors in spinal problems to include spinal surgery. This is when I came to Virginia Spine Institute for help. My doctor recalls his evaluation of my spine in early 2014:
Physician’s Perspective: I first met Mr. David McKee in February 2014. This retired Army officer presented as a referral from the doctors at Walter Reed Army Medical Center. Prior to developing neck pain and right arm numbness, he had been very active. He found that his symptoms were worse when he looked up and felt that his pain limited everything that he tried to do. He described a distribution of 30% neck pain and 70% arm symptoms.
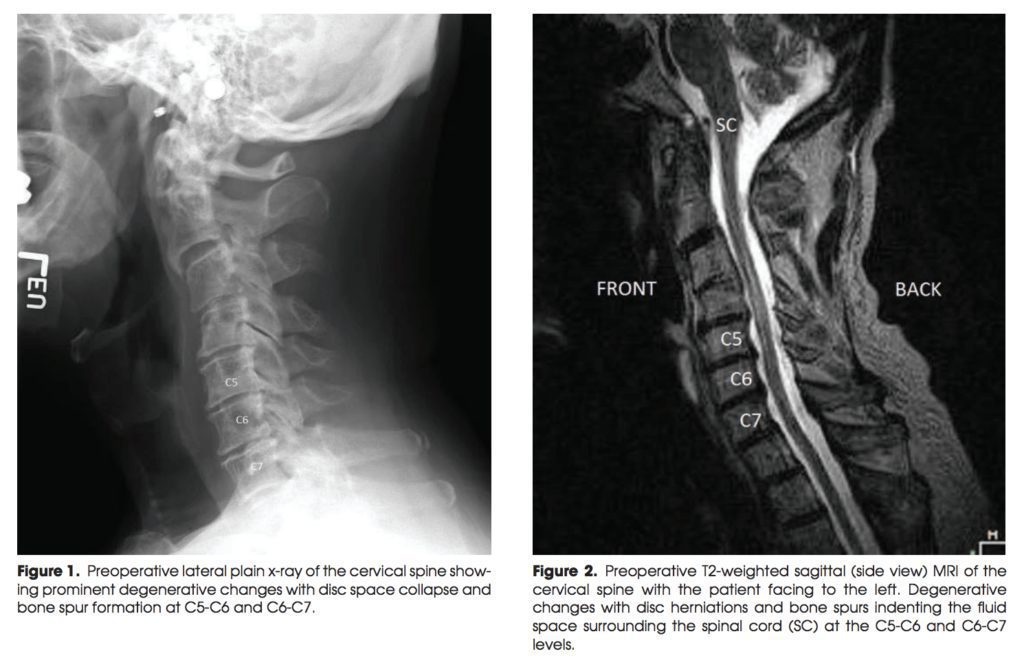
His symptoms were truly relieved by forward flexion, and he noticed some weakness in his deltoid musculature, as well as a dull ache in his upper arm and a tingling sensation in his lower forearm. He described his pain as a 4 out of 10 on a Visual Analog Scale. His imaging studies included both x-rays and an MRI scan. The x-rays showed a posture which was slightly forward flexed. He had evidence of degenerative arthritis at multiple levels and a relatively stiff spine on flexion and extension bending views. The MRI scan of the cervical spine demonstrated two areas of compression, specifically of the nerves exiting the spine and heading down his right arm.
Obviously, physical therapy would be somewhat helpful, but my concern was the weakness. Someone having evidence of irritate nerve may present as pain or numbness, but with overt weakness, my concern was loss of function. I ordered an EMG of his arms to see if there was any evidence of nerve damage.
The nerve test demonstrated signs of moderate nerve damage which appeared to be chronic, involving both the C6 and C7 distributions. In essence, there was no evidence of progressive or ongoing nerve injury, but he had clearly sustained some degree of damage. After he completed a course of physical therapy and we had a chance to review the nerve study, we decided that he was not comfortable with the degree of neck pain and upper extremity symptoms, and he wished for some relief. We discussed an anterior cervical fusion (arthrodesis) where the degenerative discs are removed, replaced with a small wedge of donor bone, and then a titanium plate is fixated across the front of the spine to promote the healing process.
David McKee: I tried the obligatory injections and physical therapy
remedies, but they were ineffective. My doctor dutifully explained that there were no guarantees with surgical remedies, and I think he was hesitant to perform surgery for someone my age, but I was almost desperate and maybe persuasive. On the 16th of April 2014, my surgery was performed and my journey to spinal health began.
Physician Perspective: In an operation lasting approximately one and one-half hour, Mr. McKee underwent anterior cervical fusion at both the C5/C6 and C6/C7 levels. There were significant bone spurs that were encroaching on the right-sided arm nerves, as well as indenting the spinal cord. He had an excellent operation with complete decompression of the spinal cord and the arm nerves on both sides. He stayed overnight in the hospital and then was discharged to home.
When I saw him back approximately two weeks after surgery, he had some mild right-sided neck pain, but the tingling that had been present previously in the right arm had resolved. We started a course of physical therapy and gave him some muscle relaxers to try to calm down the muscle spasm he was having. By July, 2014, three months after his anterior cervical fusion, he was happy. He was having no discomfort and no symptoms into his right arm, despite the EMG test showing permanent nerve damage prior to surgery.
By taking the pressure off of the nerves and stabilizing the spine, the degenerative arthritis, which was primarily causing neck pain and the irritation of the exiting nerve roots, had been stabilized. He was pleased with his progress, and at only three months after the surgery, his imaging studies were already showing signs of healing. I asked Mr. McKee to be a SpineTale because of his outstanding recovery in the early post operative period. I explained to him that it generally takes about one year for the fusion to completely heal, and many times it can take up to two years for the nerve endings to improve. He has made an outstanding recovery to this point!
David McKee: The operation was an amazing success. I’m back in the gym, back on the golf course, and back on the tennis court. Believe it or not, my tennis game is even improved – maybe because of increased flexibility. I have also returned to my other volunteer activities. And, yes, I can look at the ceiling without consequence.