Spinal Cord Injury & Stem Cells
Long gone are the days when a spinal cord injury (SCI) was a death sentence. Current medical advances allow SCI survivors to live quality lives with their injuries and prevent further health complications. In the 21st century, we are now hoping that those with SCI not only manage their disability but that they can regain motor and sensory abilities that they lost due to their injury.
Many new innovations and areas of research have ignited hope and new possibilities among SCI survivors. One of these areas of research is with cell therapy. While hesitations and objections exist and much more research is needed before cell therapy is standard of care for SCI, cell therapy is a hopeful frontier that could drastically improve a SCI survivor’s quality of life.
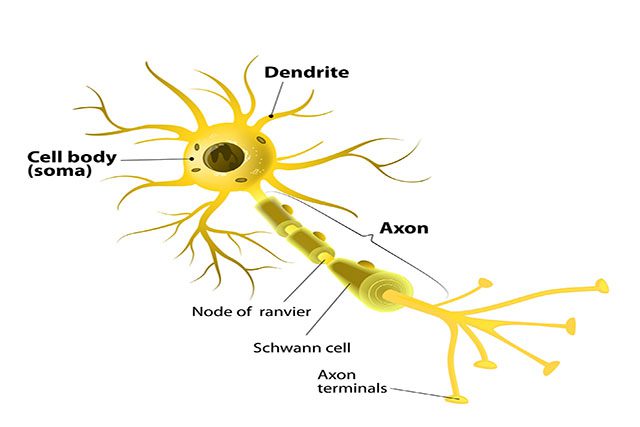
To understand the research being done with stem cells and spinal cord injuries, let’s go back to the days of biology class and refresh ourselves on the nervous system. The spinal cord has a major role in our central nervous system along with our brain. The spinal cord serves as the brain’s personal messenger to the rest of the body. Nerves extend from the spinal cord and innervate to other parts of the body (including: arms, legs, internal organs, etc.) to relay the brain’s messages. When the spinal cord is injured it can no longer serve properly as the brain’s messenger. Therefore, parts of the body can no longer function as they were meant to since they are no longer receiving messages from the spinal cord.
Depending on the location of an injury, people with a SCI might have differing levels of motor and sensory function. The use of cell therapy has the potential to return motor and sensory function. Different types of cells have been identified and research is currently being conducted to determine the effectiveness and safety of their use. The types of cells include human oligodendroctye progenitor cells, Schwann cells, bone marrow stromal cells, and nasal olfactory ensheathing cells.
Human oligodendrocyte progenitor cells, when transplanted, can spark regrowth of nerves allowing them to return to their role as messengers. This could allow function, both motor and sensory, to return. The transplantation of human oligodendrocyte progenitor cells has been found to work best when the transplant occurs soon after the initial injury.
Schwann cells (which are not stem cells) are found around the spinal cord and serve as insulation for peripheral nerves.1 When a nerve is injured, the insulation allowing for nerve conduction to occur is lost. The injection of Schwann cells helps regenerate the lost insulation around damaged areas. With Schwann cells, growth and function can continue and nerve fibers can be regenerated. The nerves are the path for messages to be sent from the spinal cord and with regeneration the message paths can be used once again. Translation: there is potential for more mobility and sensory function to return.
Bone marrow stromal cells are found inside the tissue of bones and can be injected into the fluid found around our brain and spinal cord. Clinical trials have found that the injection results in promotion of blood vessel growth. There is an initial loss of blood flow in those with SCI which results in tissue death. The injection of bone marrow stromal cells then can help recreate the communication, or nerve signaling, in injured scarred areas.1 The injection of bone marrow stromal cells then can help recreate the communication, or nerve signaling, in injured scarred areas.
Nasal olfactory ensheathing cells can also restore damaged nerves recreating the ability for messages to be sent through these nerves. This is all done from transplanting cells found in the nose into the spinal cord. It is noted from studies that these types of cells work best when the injury was recent.
Read the full article in the Spring 2015 Journal.
By Melanie Gutmann, MS