Brief Overview of Opioids
Opioids are medications used to reduce the perception of pain. The types of opioids to be aware of are:
Natural opioids – from nature, such as morphine.
Semi-synthetic opioids – modified natural opioids, such as oxycodone and hydrocodone.
Synthetic opioids – made in a lab, such as fentanyl.
Illicit opioids – any opioid used illegally, without medical oversight, or recreationally, such as heroin, street made pills, and illegally manufactured fentanyl.
Opioid pain medications work by activating the body’s natural pain-relieving receptors in the brain to decrease feelings of pain. These medications also increase dopamine, which plays a key role in reward and addiction pathways and creates feelings of euphoria.
Side Effects & Addiction Potential
Common side effects of opioids include nausea, vomiting, sleepiness, dizziness, itching, and constipation, which can lead to bowel obstructions, falls, fractures, and altered mental status. While the body can adjust to most of the side effects, constipation and itching can be persistent. The most concerning side effect is decreased respiratory drive, causing breathing to slow or stop, leading to unconsciousness and possibly death if left untreated. The risk of this is increased with higher doses of opioids or if taken with other medicines like benzodiazepines, which may be taken to control anxiety.
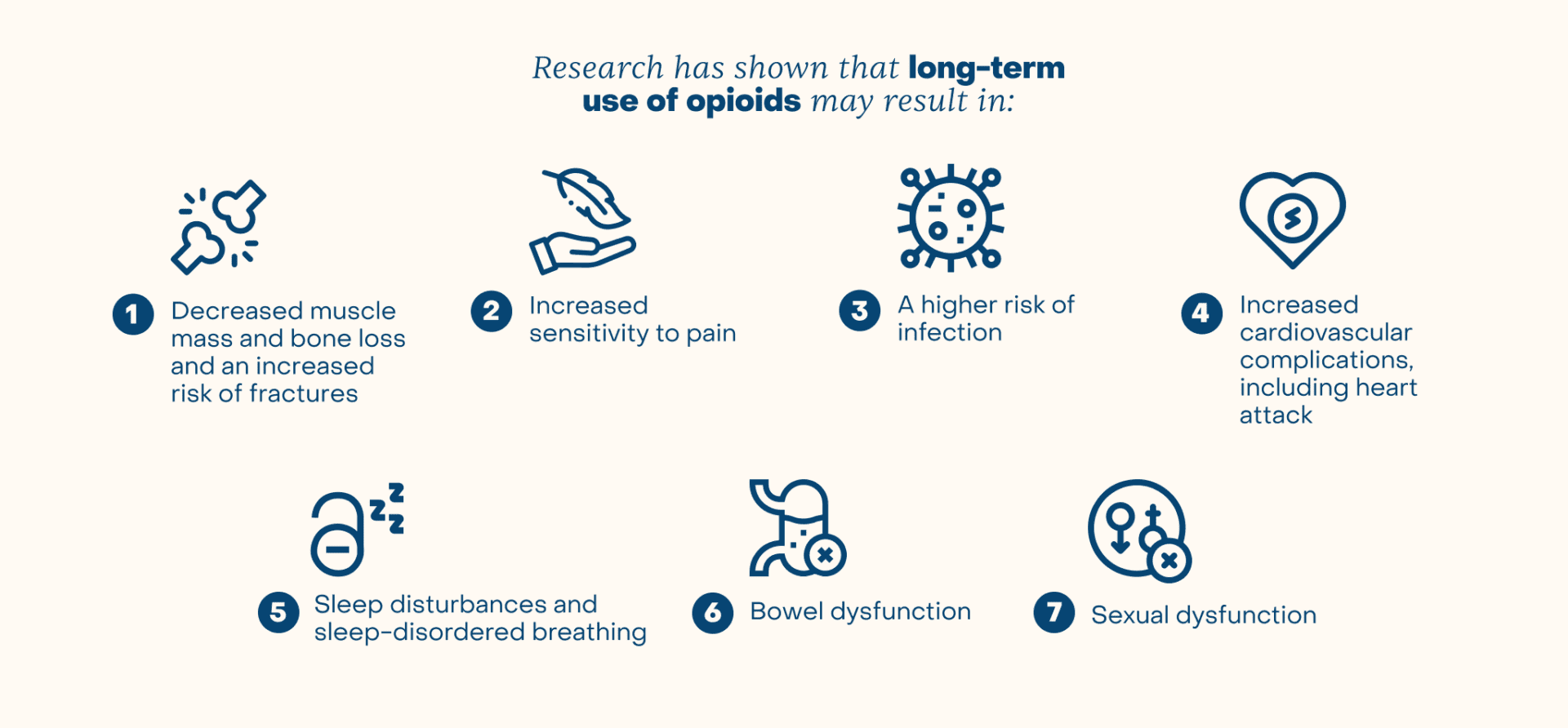
Taking opioids regularly increases the risk of developing tolerance and dependence. Opioid tolerance is the need for increased doses or more frequent doses of opioids to achieve the same effect. Physical dependence is associated with unpleasant withdrawal symptoms if the medication is stopped. While the time it takes to develop physical dependence or addiction varies by person, it can start in as little as a few weeks. Increased doses of opioids increase the risk of severe side effects while the dose required for an overdose remains the same.
The Opioid Crisis in America
The opioid epidemic has been described by the Centers for Disease Control and Prevention as a 15-year-long trend that has affected communities across the United States. This deadly crisis claimed the lives of 33,000 people in 2015. Numerous factors have been cited as playing a role in the development of this public health dilemma. In the late 1990s, The Joint Commission published rules making pain assessments part of the standard of care for every physician visit. These mandates were created due to widespread concern that pain was being undertreated. As a result of this nationally heightened awareness, pain soon became known as the “fifth vital sign.”
Although legally prescribed to treat pain, the resultant increase in prescribing patterns also increased the opioid use overall in this country, which subsequently increased the risk of abuse, misuse, dependence, and diversion. As the deaths attributed to opioids began to rise, physicians decreased their opioid prescribing patterns and illicit and synthetic variants, such as heroin and fentanyl, increased. In 2016, almost 20,000 people died from overdoses involving fentanyl and other synthetic opioids. Rural America has been most affected by the epidemic, especially the states of Kentucky, Pennsylvania, New Hampshire, Ohio and West Virginia.
When Opioids are Most & Least Effective
Opioids are used for a variety of acute and chronic conditions that cause pain. It is well understood that opioids are most effective for the treatment of acute severe pain after surgery, burns or trauma. They have also proven to be very effective for patients with terminal diseases like cancer or end-of-life palliative care. Additionally, they can be used for more specific conditions, including patients with a history of sickle cell disease who are admitted to the hospital for a vaso-occlusive crisis.
Although there are many instances when opioids can be used effectively, there are also certain clinical scenarios where they are not as beneficial. Opioids have been proven to be less effective in treating discomfort associated with neuropathic pain syndromes. These syndromes have symptoms of numbness, tingling, burning, and electric shock-like sensations that are better treated with other classes of medications that specifically target neurologic symptoms. There is limited benefit in using opioids to treat chronic pain and fibromyalgia, a pain syndrome that causes widespread, constant pain throughout the body. Opioids are also known to be less efficacious in the treatment of headaches and migraines, as they can increase the risk for medication overuse headaches or chronic migraines.
Conclusion
In conclusion, opioids are best used under direct medical supervision for conditions that have been shown to be effectively treated with opioids. These medications should be used at the lowest possible dose to be effective and for the shortest duration necessary. Non-opioid medications and other therapies to reduce pain are alternatives that can have great benefits to those in pain.
¹ Centers for Disease Control and Prevention. Opioid Overdose—Understanding the Epidemic. https://www.cdc.gov/drugoverdose/epidemic/ index.html.
² Centers for Disease Control and Prevention. Opioid Overdose—Fentanyl. https://www.cdc.gov/drugoverdose/opioids/fentanyl.html.



