At the National Spine Health Foundation, we love to share the stories of patients and Spinal Champions who have overcome their back and neck pain issues in a way that gives them their lives back. You can read more about our Spinal Champion® program here. Now, on to Lauren’s incredible story of lumbar spine surgery success.
Lauren’s Story: In Her Words
My back pain first started while I was on a band trip to Florida during my sophomore year of high school. I learned you could go to the front of the line at Disney World if you’re in a wheel chair. After my trip, my primary care physician ordered x-rays and instructed me to take some muscle relaxers and rest. Unfortunately, the x-rays were inconclusive, but the pain continued to get worse. A few months later, I had an MRI done, and after reviewing the results, my doctor recommended I go see a specialist. The orthopedic surgeon told me and my parents, who went with me to all my appointments, that she didn’t know how I was able to walk around due to a very large disc herniation.
When she asked what I had done to cause this large two level herniation in my lower back, I had no answer. I hadn’t been in a car wreck or done anything that could have caused this horrible pain. It had come on gradually and got progressively worse as time went on. The doctor felt that I needed to have surgery immediately, and we scheduled my first back operation ten days from that appointment. Not long after, my herniation had reoccurred, requiring a second surgery that was performed by a neurosurgeon; much physical therapy was required for my recovery.
Post-Surgery Struggles
I was able to walk across the stage to receive my high school graduation diploma and made plans to begin college in the fall. My parents felt it was important for me to stay close to home because I was still having back pain and continued to see the neurosurgeon for checkups. I was learning to live with constant pain, thinking it would always be something I would have to put up with everyday.
As I entered my second year of college, the pain I had been trying to ignore was starting to cause me to spend more and more time in bed when not in class. I decided the pain was becoming unbearable again. After reviewing another set of MRI’s, the doctor said the herniation was so severe that he was very concerned I could suffer drop foot. This time the surgeon wanted to perform two new tests, an EMG study and a CT scan. The first test they’d done that day didn’t show anything severe enough to be causing me that much pain. He called back the next day, reporting that the second test showed severe damage requiring yet another surgery. Trying to express to others the intense pain I was in when it’s not something they can visibly see always made me feel that people thought I was overreacting. The frustration and doubts were another set of symptoms that accompanied the pain.
A few years after my third surgery I was still living with pain and taking medication daily, but I tried once again to move on with my life. When I wasn’t working, I would be in my bed trying to find any relief I could. I couldn’t hang out or take road trips with friends; the pain would just get too overwhelming. My parents were beside themselves watching me deal with all this, and feeling frustrated that we could find no solution to alleviate this life altering pain.
Seeking a Solution: Neck Pain Arises
Our next effort was to get a consultation at a reputable facility. I had a great doctor who was very kind, and I felt I had a good connection with him. He said he would operate once again, but still could not give us any guarantee that this would take away the pain. After the surgery, I had finally experienced relief from the constant pain. I was so excited and hopeful that I could finally have an almost normal life. I would always have some pain, but maybe this time it wouldn’t become so extreme.
I had about six wonderful months before the pain started coming back once again. During this time, I was diagnosed with fibromyalgia, a chronic pain disorder, and a new cocktail of pills prescribed by a rheumatologist was added to my daily intake of medication. I had also developed persistent neck pain after the third surgery.
>>>>>> Dennis’ Extreme Obstacle Course Races Post-Fusion
One of my mom’s friends recommended the Virginia Spine Institute. Anyone who has seen Dr. Subach knows what a fun sense of humor he has, but also how he listens to what you have to say. He doesn’t talk down to you or make you feel that what you are dealing with can’t be as bad as you describe it. He, along with his wonderful physician assistants truly make you feel that you are in good hands.
This time, the problem would require neck surgery. You would think that after all the failed back surgeries, I wouldn’t think of going through it again with my neck, but I really trusted Dr. Subach and his plan for taking away this pain. I am happy to say he was successful! It was amazing how much better my neck felt after a two-level fusion surgery. To this day, my neck is still not causing me that initial pain I was going through.
After my neck pain had been relieved, I once again was back at the drawing board to address my continued back pain. I started to go though different tests and MRI’s to find out the current condition of my back. Dr. Subach felt that there was a lot of scar tissue and doing another surgery wasn’t going to fix the problem.
After nearly nine years of constant pain, little to no exercise, and extended periods of bed rest, I had gained a lot of weight. I repeatedly heard that losing weight would help with the back pain, but despite trying numerous weight loss plans, nothing seemed to help. In addition to the ongoing deep depression I had been dealing with, losing weight was not something I was able to do on my own.
Weight Loss and Disability
In the next chapter of my life, I was found eligible for disability. That process took over two years to be approved and included a lot of stress and court appointments. However, once that process was completed, I then had Medicare which thankfully would pay for gastric bypass surgery, something Dr. Subach had recommended. This was the most painful recovery I have ever been through in my life; not only was my back in constant pain, but my abdominal area was in horrendous pain from the bypass procedure. Eventually I was able to start walking and doing a little exercising.
As the months went by, I was amazed to see a totally different person looking back at me in the mirror. On the one year anniversary of the bypass surgery, I had lost a total of 170 pounds since my initial visit to the doctor. Feeling better about myself helped take away some of the depression and anxiety I had been going through, but I still had nonstop back pain and returned to Dr. Subach’s office for a consultation.
Looking Towards Lumbar Spine Surgery
Dr. Subach recounts his clinical evaluation of my lumbar spine:
“Lauren had been suffering from back and bilateral leg weakness and numbness for the past ten years. When asked to grade her pain, she stated that it was a nine on a visual analog scale of ten in terms of severity. She reported that there were no specific injuries which lead to this, however, spinal disorders did run in her family.
The EMG study of her legs demonstrated not only the presence of chronic nerve damage in the right L5 and S1 nerve distributions, but also acute denervation of moderate severity in both of those nerves as well. Her lumbar MRI scan and x-rays demonstrated obvious degenerative changes involving the L3/L4, L4/L5, and L5/S1 disc spaces with evidence of a mobile spondylolisthesis at L3/L4. She underwent lumbar discog- raphy to better evaluate the disc spaces and there was evidence of concordant and positive pain reproduction from L2/L3, L3/L4, L4/L5, and L5/S1 with obvious degenerative changes at each level.
Having had previous lumbar spinal surgery with evidence of instability at L3/L4 along with evidence of progressive nerve damage at L5 and S1, she was a candidate for additional spinal surgery. In general, when the problem is compression of the nerves and in- stability, it requires a decompression and stabilization operation. We discussed the options, including anterior lumbar surgery and posterior lumbar surgery. Although it would be a significant operation, her quality of life was such that she could not exist without pain medications, and she was essentially disabled because of the discomfort.”
Dr. Subach and his team spent a lot of time talking about the pros and cons of going through this type of surgery. Over and over again, I was told that it may not fix the pain, it might even be worse afterwards. Once again, I had such faith in Dr. Subach that I felt I needed to try this last (hopefully) procedure which might give me a chance of a normal life if it worked.
Lumbar Spine Surgery Operation and Recovery
Dr. Subach’s explains my operation and recovery:
“In conjunction with her family, she made the decision to pursue operative intervention and under- went surgery in September 2012. The surgery that she underwent, called a transforaminal lumbar interbody fusion (TLIF), at the L3/L4, L4/L5, and L5/S1 levels involved removing each of the degenerative discs, restoring disc space height and normal posture with devices placed into the disc spaces, and decompressing each of the spinal nerves, particularly the right L5 and S1 nerve roots which were showing evidence of progressive damage.
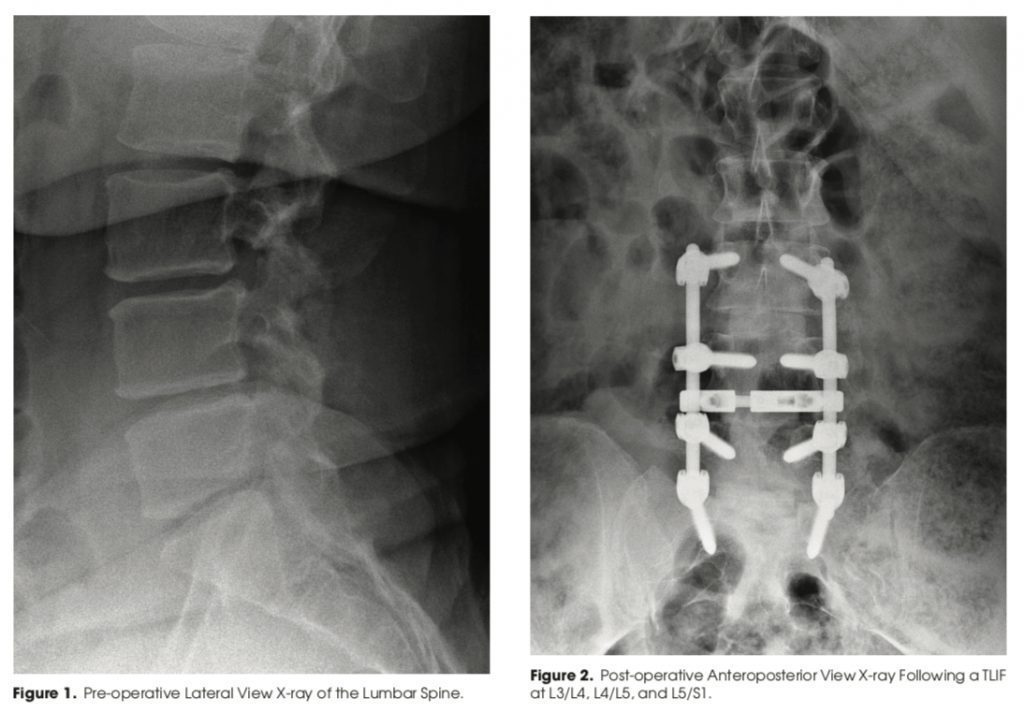
In a four-hour operation requiring a few days of recovery in the hospital, Lauren tolerated the operation extremely well and was sore; however, she noticed that her back felt stronger immediately.
When I saw her at two weeks after surgery, her pain level was down to a two on a scale of ten. She continued to have some mild discomfort and some numb sensation in the legs, but she felt that she was already doing better than she was prior to surgery despite the size of the intervention. By June 2013, nine months out from the surgery, she had continued mild discomfort around the area of her incision most likely related to the hardware, specifically with increasing activity. Overall, she was much improved.
Lauren had undergone four previous surgical interventions prior to this extensive reconstruction procedure. She is now able to exercise and be more active, and, for the first time, she feels that she has her life back. Not only does credit go to Lauren, but also her family who was a significant support system throughout the previous operations as well as this more recent procedure.”
Lauren’s Conclusion: A Spinal Champion®
While I may not be able to do the limbo, my back feels so much better. I can’t believe it’s true. I really don’t know how I survived all those years with the excruciating pain. I am so thankful for everything Dr. Subach and his team have done for me. I am now able to do all the things I missed out on over the past ten years; I’ve ridden in my brother’s race car during a drifting event, gone tubing down the river, driven for hours in the car enjoying road trips, taken long walks on the Manassas battlefields with my dog, and participated in life like I was never able to do before.
Looking for more inspirational stories? Or want to share your own success story? Check out our Spinal Champion® program to share and find more stories of hope!