Q1: Where are stem cells sourced?
Research and development of stem cells has been an exciting new development as a potential treatment for many conditions that were previously considered incurable. Stem cell research for the spine (and in general) has hit its stride since the late 1990’s, both in terms of basic research as well as various clinical applications. In fact, there are several diseases for which stem cell treatment is rapidly becoming a viable treatment option.
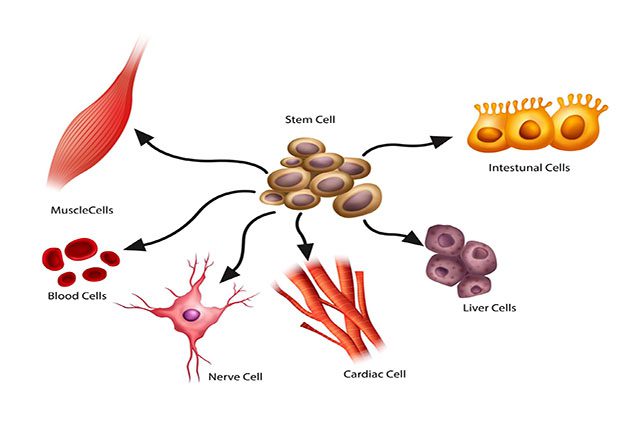
A “stem cell” by definition has two important characteristics: the ability to self-replicate to create more stem cells (like the parent cell) and the capability to mature (in the right environment) into any particular mature cell type of a human body (pluripotency).
Stem cells are derived from various sources. For example, embryonic stem cells (ESCs) are derived from embryos; mesenchymal stem cells (MSCs) can be sourced from bone marrow, adipose tissue, and umbilical cord tissue to name a few; organ-specific stem cells are derived from specialized tissue (e.g. neuro stem cells (NSCs)); induced pluripotent stem cells (iPSCs) are stem cells that are generated from reprogrammed mature cells. The original research that looked into the possibility of using stem cells as therapeutic tools focused on ESCs. These are stem cells derived from otherwise nonviable embryos. While many consider ESCs to be the best sourcing option, ethical issues continue to be a major factor in both funding basic research into ESCs as well as their translational applications. In 2001, the federal government under President George W. Bush restricted federal grant mechanisms to the research and applications to those embryotic stem cell lines that were already in existence at that time.
Since 2001, there have been various other modalities, including deriving more “mature” stem cells from each part of the human body (such as deriving organ specific stem cells from adult animals). Central to this approach has been the discovery by several groups of researchers that all adult mammals harbor organ-specific stem cells in the mature state (like NSC in the brain and spinal cord, etc.) MSCs are derived from the bone marrow. Intrinsically, MSCs are thought by some to have pluripotent properties like ESCs. Additionally, many researchers have been able to reprogram these stem cells to drive differentiation and maturation into mature cells of other organ systems.
Approximately six to seven years ago, a more exciting development took place. Researchers at the University of Wisconsin, Madison, and subsequently other locations were able to synthesize stem cells by reprogramming mature cells in the reverse direction such that they could take on stem cell-like properties. These so-called iPSCs, while still in the early stages of research, represent a significant solution for future cellular engineering and derivation of stem cell populations without ethical issues.
Q2: How is stem cell research regulated?
Stem cell research is heavily regulated in the United States, especially the efforts funded by federal grants. As noted above, stem cells by virtue of their pluripotency can have significant potential adverse effects after transplantation, principal among these being the formation of cancerous cells. Therefore, the FDA (Food & Drug Administration) has established strict guidelines in terms of conducting clinical trials that use stem cells that are considered to have significant treatment potential.
In general, stem cell research is subjected to very high standards of ethical scrutiny. Most institutions, both academic and private, have a cross-sectional regulatory panel that reviews and approves stem cell research projects. These panels are typically composed of stem cell researchers, ethicists, lay individuals from local communities, and individuals with legal and regulatory expertise.
Q3: Is stem cell treatment for spine safe and effective?
Currently, stem cell treatments for spine problems, specifically for spinal cord injury, are in the early stages. To date, there have been very few clinical trials in the United States that look at the potential of stem cells for treating spinal cord injury. The first Phase I trial, sponsored by GERON Corporation, began in 2009 and involved the transplantation of embryonic-derived stem cells into patients with acute spinal cord injury. This study was terminated after approximately five patients were treated with transplanted cells due to funding concerns. More recently, Stem Cells Inc. has begun another study transplanting stem cells for chronic spinal cord injury (four months to two years after injury). While these studies have so far shown no untoward effects of stem cells after transplantation into the spinal cord, the therapeutic benefits are yet to be fully understood.
Elsewhere in the world, there have been many attempts to perform clinical studies with stem cells, mostly in China and Korea. These include ESCs and umbilical cord-derived stem cells as treatment modalities. These studies are being done with guidance from experienced researchers worldwide and are still in their early stages of performance. Results as to the benefit of such stem cell transplants are not yet available.
Q4: What are the different potential applications for stem cells in spine treatment?
The applications and current state of stem cells for the treatment of spinal cord injury are noted above. Other spinal applications for stem cell research and eventually treatments include the use of stem cells for improving the grade of spinal fusion surgery, with efforts to regenerate other types of spinal supportive tissue, including ligaments as well as joints, and finally, for the regeneration of intervertebral discs in the lumbar or cervical spine. Disc degeneration and disc herniations affect 80% of Americans. These afflictions are a common problem that affects quality of life by causing back and neck pain, arm and leg weakness, and therefore are a significant source of lack of productivity in the workforce. Stem cell treatments developed to regenerate and/or repair degenerated discs would be of great benefit in the future.
Q5: How are donor stem cells matched to the patient for transplantation?
In general, stem cells are transplanted under cover of immunosuppression, much like a patient receiving a liver or a kidney transplant. The duration of immunosuppressive treatment after transplantation can last from several weeks after the transplantation procedure has been completed and sometimes for life, as in solid organ transplants. One of the most significant efforts in stem cell research has been to generate MSCs as described in response to Question #1. MSC transplants would involve developing the patient’s own stem cells, thus obviating the need for immunosuppression. iPSCs, if developed for viable clinical application, would also eliminate the need for immunosuppressants.
By Shekar N. Kurpad, MD, PhD