“Oh no, I cannot believe it! My doctor just used the F word!?!!?”
“I have got to get out of here, this guy must be crazy! Oh my God, this is the end of my life! I will never be able to do anything again…”
This reaction is an all too common and, in many cases, an unnecessary first reaction many patients have when speaking to their doctor about a spinal fusion. Let’s face it, we all would like to live our lives without needing surgery and especially a spinal surgery. That being said, for some patients with spinal conditions, their lives can be much better after having a spinal fusion than they would have been without a spinal fusion.
There is a great deal of misinformation on the internet and in the media about spinal surgery and specifically spinal fusion. When contemplating a spinal surgery and deciding if a fusion is necessary, it is critical to consider multiple factors. First and foremost, the vast majority of patients with a spine problem can be successfully treated and live a good quality of life without ever undergoing a spinal surgery.
Many patients who I see who are coming in for a surgical opinion after having “failed non- operative treatment;” they actually are able to improve once a proper non-operative course is initiated and maintained. Modern spinal health care can successfully treat most patients through a combination of exercise, therapy, spinal manipulation, medications, and non-operative procedures such as spinal injections or regenerative treatments like prolotherapy, PRP, or stem cells.
The decision to contemplate a spinal surgery depends not only on what kind of problem is happening in the spine, but more importantly what kind of pain and limitation it is causing the person in his or her life. The decision to consider surgery, especially a fusion, should be made mainly based on a patient’s symptoms and quality of life rather than on pictures from an MRI scan or an x-ray.
For certain patients with specific structural problems in their spine that are causing severe pain or limitation in quality of life or danger for the future, spinal surgery offers an option that can lead to a much better quality of life than living with the current condition and symptom.
There are certain problems that develop in the spine that can be treated surgically without requiring fusion and in those cases, that treatment option is preferable to fusion.
If you think about the anatomy of the spine, it is a series of bones and discs stacked one on top of another. The purpose of the discs is to hold the bones apart, providing a cushioning effect. These bones and discs are attached by muscles and ligaments, and these structures all move together as a person is active throughout the course of his or her life. I sometimes use the example of cars on a roller coaster, all attached together but with movement between each level. The discs cushion the bones and prevent friction and also hold the bones apart, which maintain a space for the nerves, which run inside the spine. The spinal cord branches off of the brain and runs down into the neck. The spinal cord and the nerves of the spine run inside the bones of the spine much like a cable in a conduit pipe. At each disc level, nerves branch out.
In the neck, the spinal cord and nerves branch of the brain and run down inside the spine like a cable in a conduit pipe. Nerves branch out of the spine through small holes at each disc level and run to the body like little electrical cables. If someone develops a problem with the nerve in the spine, they can develop symptoms anywhere where that nerve runs, including pain, pins and needles, burning, numbness, or weakness.
For some conditions, when a nerve is pinched or a small amount of arthritis develops, minimally invasive surgeries to “unpinch” a nerve or “shave a bone spur away” may be effective at alleviating a patient’s symptoms without moving forward to a spinal fusion. These are especially good options for patient who have pain mainly related to a pinched nerve (arm
or leg pain). These procedures can be performed through very small incisions using a microscope or fiber optics.

Spinal fusion involves using some form of implants (metal, plastic, bone) to hold two of the bones of the spine together and use bone graft to weld those two bones together. A good analogy is to think of placing cement or grout between the two bones, which ultimately hardens, much like a broken bone mending in a cast. Once this process occurs, those two bones are now welded into one solid piece (a fusion), and that level of the spine is never able to move again. This does take away the motion of the spine at that location.
Obviously, when a fusion is performed, the trade-off is that particular level of the spine is not able to move any more. For some patients, this is actually a good trade off because a fusion is a way to treat pathologic motion or instability in the back. For patients with spinal instability, if surgery is needed, a fusion is almost always the best option.
Conditions That Can Develop
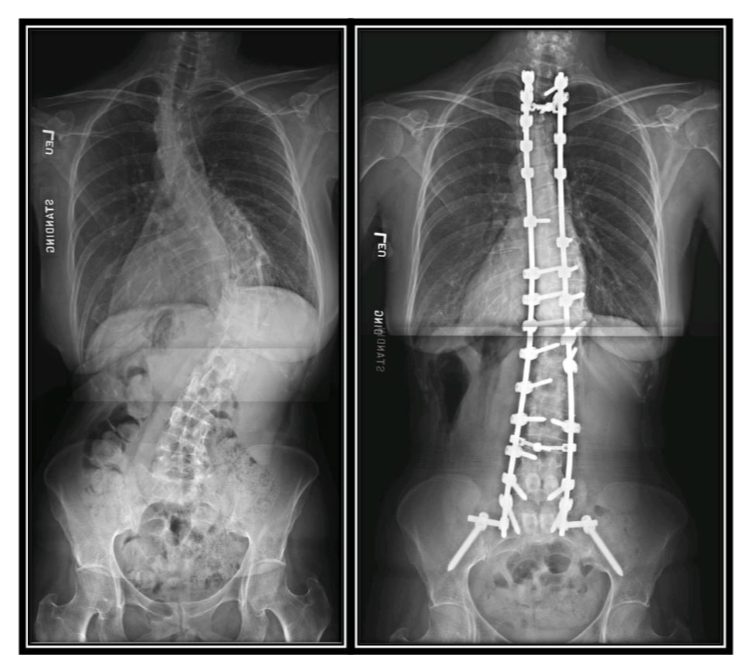
Many patients develop spondylolisthesis (an instability with slippage of one bone on top of another in the spine) or scoliosis. For patients these problems, malalignment and instability between the bones of the spine is a large cause of the patient’s pain and the only way to alleviate this instability with surgery is to realign and fuse the bones together. In a situation where a patient has a spinal deformity or instability, any surgical option that does not provide stability does not have a good chance of improving the pain and has a high likelihood that the condition will continue to worsen in the future. As of today, options to hold the spine bones without actually fusing them are not a good option because as time passes and the spine continues to move, those implants eventually work loose and cause even bigger problems.
Other conditions that commonly require spinal fusion include fractures or tumors where a tumor actually destroys a bone of the spine creating a spinal instability.
I commonly hear stories from patients about a friend or a relative who has undergone a spinal fusion and how the surgery has helped or not helped them. I am always trying to help people understand that two different patients with two different fusions may have completely different problems and completely different rates of success.
For many spinal conditions, the type of problem that is causing the symptoms is a big predictor of how well the patient will do in the future with or without surgery. It makes sense if you think about it, the worse your problem is at the beginning, the harder it may be to deal with.
Patients who have healthy discs and bones all throughout their spine, with the exception of one injured disc, have a much different prognosis with or without surgery than patients who have degenerated or injured discs at every level in the spine. Again, the better off you are at the beginning, the better off you are likely to be at the end of treatment.
Different Kinds of Fusions
When we think about it, it seems very intuitive that a person undergoing a one level fusion would have a very different surgery and recovery than a patient undergoing a five level fusion. Obviously, if a person needs surgery we would always prefer for them to need a very small and successful surgery, but we are forced to treat the type of problem that a specific patient has, and for patients with more severe spinal problem, this may require a more involved surgical treatment.
In some cases, “bigger spine surgeries” are actually the ones that can help a patient’s life to improve the most because the condition they are starting with is so much more limiting and dangerous.
I have a very well connected patient who had a disc herniation in his back some years ago causing a pinched nerve. He had severe pain for over one year before deciding to have surgery, but eventually elected to undergo a lumbar microdiscectomy (a minimally invasive non-fusion surgery performed through a skin incision less than inch long). He has done phenomenally well and ultimately has referred many other patients to me. They always come to me and say they want the surgery that “Jim had.” “Jim” has told them all about his surgery and how well he has done, and they are hoping to be as lucky as “Jim.”
I then have to spend a good deal of time helping them to understand how the problem that is taking place in their back may or may not be similar to the one in “Jim’s back.” For me, it has been very important for them to understand how their problem is different than “Jim’s,” and, therefore, why their treatment will also be different.
Another reason it is very difficult for patients to compare the success of their treatments is also because of how differently people may respond to surgical treatment. It is not just the type of spinal problem or the number of levels affected, things such as general health, level of physical fitness, pain tolerance, smoking, mental health, and motivation all play a critical role in determining how someone will recover from any surgical procedure and in helping to predict what their chances of success are after a surgical procedure.
More Severe Spinal Problems
For patients starting with a much more severe spinal problem, particularly patients who have many other medical problems and may be severely disabled because of them, how we define success or what type of activities or quality of life we may be able to get them back to may be different than someone who is younger and healthy with a simpler spinal problem.
Think of contracting with a building company to renovate your house. If you live on a nice piece of property and your old house is in relatively good shape, you have a good chance of coming through your renovation on time and on budget. On the other hand, if your land is contaminated with an oil leak and the entire house is falling down and the foundation is eroded, you are very likely to get into some unforeseen problems during the renovation that will cause your renovation to take much longer than expected and go way over budget.
In the end, the total improvement you can achieve is actually higher on the second property, but it takes a lot more work to get there. When it comes to spinal fusions, even for the same condition and for similar patients, it is critical to note that all spinal fusions are not created equal.
There are many ways to go about fusing a single level of the spine, mainly related to the direction that the surgeon uses to approach the spine and the amount of damage this may cause to the body on the way in. In general, a surgeon can reach a person’s spine through the back (posterior), the front (anterior), the side (lateral), or some combination of these approaches. There are also many different types of implants and grafts used to achieve fusion and these can play a major role in determining success versus failure.
When performing surgery, our goal is get to the body part that is diseased while trying to avoid disrupting or damaging normal body tissues on
the way in and the way out. Surgery in the back portion of the spine carries a different level of pain and disruption of normal tissues than does surgery in the side or the front. Ideally, the approach a surgeon uses to fix a problem should depend on the exact location of the problem for the patient, but in many cases, the approach a surgeon uses may be based simply on their education, preference, convenience, or comfort level.
When contemplating a spinal fusion, I believe it is critical to work with a surgeon who is comfortable with every approach and can factor in the benefits and risks of each approach when making a recommendation. Surgeons who are not trained or do not commonly use each approach are very limited in what they can offer a patient. I remember the old adage, “if the only tool in your toolbox is a hammer, everything looks like a nail.” If a surgeon only does surgery through an incision in the back of the spine, then that is the only type of surgery they will recommend.
A Final, Critical Component
A final critical component to a successful spinal fusion is in the postoperative recovery period. Spinal fusions take time for the bones to weld together, just like a broken bone healing in a cast. During this critical time, moving, bending, twisting, and using those bones too aggressively can prevent the spinal fusion from healing, thereby decreasing the chances of success. When I see patients who have had failure after a spinal fusion, in many cases, it can be linked to some problem that occurred during the early healing period. In some cases this is because the patient was not properly warned about the healing precautions and in some cases it is because the patient could not or would not follow the precautions.
If you are going to go through a spinal fusion, it is critical to do everything in the recovery time to make sure that it has the highest chance of healing well. On average, spinal fusions in the low back take approximately three months to become strong enough for people to return to heavy physical activities.
Quite simply put, using nicotine is the worst thing you can do to your spine. Smoking kills the little blood vessels that deliver oxygen to your body causing you to age faster. Smoking kills your discs causing back pain. Smoking also increases the receptors in your brain that cause you to feel pain. YES, SMOKING IS CAUSING YOUR BACK TO HURT YOU MORE.
Finally, smoking prevents the body from healing and if people use nicotine around the time of surgery, they have much higher rates of wound infection, failure of fusion, medical complications, and chronic pain. If you are going to have a spine surgery, you need to do everything you can to make it a success. NOT using nicotine is absolutely the most important thing you can do to help you spine now and in the future. Please, if you are going to do one thing after reading this article, consider quitting.
Clearing up Misunderstanding
A very common interpretation in the public is that if a person has to have a spinal fusion, it will rapidly lead to the deterioration of the other levels in the back requiring more surgery. There is some truth to this concern but also a lot of misunderstanding. In the low back, there are six discs in the average patient, all sharing the load as the low back bends and lifts and twists throughout the course of life. All of us are sustaining a slow degeneration of our discs over time as part of the natural aging process.
If a person loses a disc through arthritis or a surgical fusion and that level is no longer moving, then the remaining discs are all seeing a partial increase in stress as they pick up the slack. In this situation, the remaining disc may actually degenerate even faster than they already were going to. If a patient needs a surgery, the approach used to perform the fusion and the amount of disruption and damage to the remaining structures in the spine can also play a critical role in determining how long the remaining discs last before they go out.
Many studies looking at older surgical techniques showed very high rates of disc disease requiring fusion at levels above a spinal fusion. None of these studies ever commented on the health of the other discs before the initial surgery, and the chances are that many of the discs were going bad even before the initial fusion. In these studies, the most common surgical technique used was a very large incision on the back of the spine, which involved detaching all of the spinal muscles and ligaments, and it is understandable how this, coupled with the loss of motion at the fusion, could speed along disc problems at other levels. Using newer (and better) surgical techniques that are minimally invasive, less disruptive, and more protective to tissues, these rates of adjacent segment degeneration are much lower but are still an important consideration.
There is, however, another very important factor to consider that is rarely discussed. These days, if a person has to have a fusion, essentially everything else that happens in the spine after that is always blamed on the fusion. In reality, many of these problems were likely already going to happen whether a fusion was performed or not. For many patients, disc problems come from a combination of genetics and the stress they may put on their discs throughout their life. Genetics play a very important role in determining how long your discs are going to last. This is why some people are able to play contact sports throughout their whole life without having any issues, whereas some people develop major disc problems with relatively low stress physical activities. It is true that the wear and tear plays an important role, but for many people, their disc disease is genetically programmed.
I commonly compare progressive degenerative disc disease with the process of developing gray hair or going bald. There is a genetic reason why one man will start to lose his hair in his twenties while another will have a full head of hair through his entire life. This is based on genetics and inherited through your genes. That is why baldness, grey hair, disc disease, and many other conditions tend to run in families.
If you think of a patient who has a genetic predisposition to degenerative disc disease, all of their discs are programmed to wear out at an earlier rate. In that patient, if one disc develops a severe problem requiring surgery, then surgery at that location will not do anything to prevent the patient from continuing to develop disc problems at their other degenerating levels. If that patient needs a fusion, then the fusion is later blamed on whatever may happen, when the reality is that even if the surgeon could replace that bad disc with a magic wand, the other discs will continue to degenerate as they have already started.

As a surgeon, I always try to avoid fusion when it is the right thing for a patient, but when I have to do a fusion, I try to help the patient understand this fact, and I try to perform the fusion in the safest possible way to protect the remainder of the back in the years down the road.
Nobody wants to have surgery. Trust me, I understand. That being said, for some patients with some conditions, spinal fusion allows a much better quality of life and level of activity than leaving the problem untreated. For patients who are lucky enough to be in very good shape and have one or two level spinal problems, many are able to return to a very high level of physical activity and a normal life.
I personally believe it is very important for your surgeon to understand you, your job, your family, your priorities and values, and your quality of life. The doctor understanding just your MRI is not enough to make the best recommendation for any given patient. One shoe does NOT fit all.
A Better Future in Store
For patients with more severe spinal problems, such as, multilevel genetic spinal degeneration, severe spinal curvatures and instabilities, spinal surgery with fusion can provide a much better future than mother nature had in store for the patient, even though for someone in this scenario, the trade-off of the spinal fusion may leave them with less motion than someone with a “normal back.” For someone in this scenario, they are starting with a very abnormal back, and while the fusion can make them much better, it cannot restore a normal back to someone who did not have one to start with.
If you are contemplating a spinal surgery or a spinal fusion, it is critical to understand the type of problem that you have, the type of patient that you are, and how the particular surgery that could be used to help your problem may or may not allow you to do the things that you love. We all have to make choices in life and the majority of patients who correctly receive a spinal fusion can expect to have a much better quality of life than they would have had without surgery.
If your spinal problem is limiting your quality of life in a way that is unacceptable to you and the surgery that could be used to fix it has a high chance of giving you a better level of function and quality of life, then a spinal fusion may be the right choice for you. If a fusion is going to be performed, it is critical to get it done right the first time and that it is performed in the least invasive fashion. It is equally important that you to do everything needed in the recovery period to make sure that the fusion heals properly and then you have to keep your body as healthy and as strong as possible to protect the remaining portions of your spine in the future.

Dr. Christopher Good is President of Virginia Spine Institute and a Board Member of the National Spine Health Foundation. He is also a member of our Medical & Scientific Board.