Emerging Imaging in Muscoloskeltal Medicine
Since the discovery of x-rays in the late 1800s, there have been substantial advances in the field of musculoskeletal imaging. So, just what is this type of imaging? Well, for starters, it involves the diagnostic evaluation of the musculoskeletal anatomy.
The initial use of x-rays, as far back as the 1890s, was to assess for broken bones; however, the subsequent development of both computerized tomography (CT scans) and magnetic resonance imaging (MRIs) allowed for a better and more sensitive evaluation of the musculoskeletal system. More recently, ultrasound has emerged and gained widespread acceptance for the evaluation of the musculoskeletal system. Diagnostic ultrasound has its origin in sound navigation and ranging (SONAR) and involves oscillating sound pressure waves to visualize muscles, tendons, and many of our internal organs. Musculoskeletal ultrasound can serve as an excellent diagnostic modality for a musculoskeletal physician. The structures which are commonly and easily visualized as well as evaluated include: tendons, nerves, muscles, and osseous structures.
Although an MRI is much more frequently ordered, each imaging study has its advantages and disadvantages. Ultrasound has significant benefits and has one particular advantage over an MRI – in that it is much less expensive. It is also much more patient friendly and more easily tolerated compared to an MRI. Claustrophobia is commonly encountered with MRI scans and is not encountered in an ultrasound examination. MRI and ultrasound can both examine large areas of the body with extended field of view; however, ultrasound examinations are dynamic studies. For example, the affected part can be imaged in real time, observing for pathologic movement in tendon, bursa, muscles, or joints. MRI does not allow for this and only provides a static picture of the anatomy. Since the ultrasound evaluation is dynamic, the structures evaluated can be changed and revised during the study based on results. Ultrasound evaluations also allow for immediate results, and that in turn allows for treatment plans to be developed at the time of imaging.
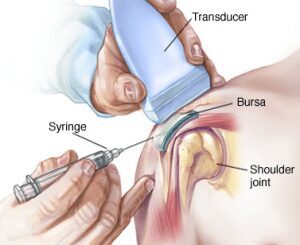
Ultrasound can also be utilized for interventional procedures. Compared to the use of fluoroscopic and CT guidance, ultrasound has many advantages. Fluoroscopic and CT guidance are currently the most frequently modalities used to localize needle placement during an interventional treatments such as a tendon injection. Both of these modalities use ionizing radiation to visualize structures. Fluoroscopy does not visualize soft tissues, but instead relies on bony landmarks and often necessitates iodinated contrast dye in order to prevent inadvertent intravascular placement and to confirm placement. Contrast dye is used to assess placement of the needle in soft tissue, but some patients may be allergic to contrast and would need prophylactic medication to prevent a reaction. Ultrasound, on the other hand, does not utilize ionizing radiation, so contrast would not be needed. And thus, various soft tissues and joints can be directly entered, aspirated, or drained. It has been estimated that approximately 29% of knee injections may miss the joint without guidance. However, with the use of ultrasound guidance, the needle can be visualized when entering the joint space.
It is important to note that diagnostic ultrasound has many limitations as well. It is dependent on body habitus, and in certain situations, it may not be able to penetrate excessive soft tissue in order to evaluate deep structures. The benefit of the ultrasound evaluation is operator dependent and requires performance by an experienced clinician. Without this, optimal image acquisition will not be obtained, and pathology may be missed or misinterpreted.
There are current estimates stating that approximately 30% of all musculoskeletal injuries are muscular; ultrasound is an excellent imaging modality to detect and classify these types of injuries. Injuries such as rotator cuff tears, hamstring tears, and other muscular injuries can be detected using this diagnostic study. MRI is the most useful modality when assessing joint pathology; however, ultrasound is the best diagnostic modality to assess for joint effusions. Nerves can also be studied using diagnostic ultrasound. Nerve impingements such as carpal tunnel syndrome can be directly visualized to assess the severity of the impingement.
Diagnostic ultrasound is an excellent imaging modality to assess musculoskeletal pathology, yet it is often under-used. Recent improvements and advances in ultrasound technology make it much more accurate and dynamic than other modalities such as CT and MRI. Ultrasound is easily tolerated, low cost, and highly dynamic and portable which makes it an ideal modality for musculoskeletal physicians to use in diagnostic and interventional purposes.

Niteesh Bharara, MD, DABPMR
Virginia Spine Institute