The Future of Spine Surgery
The modern goals of the future of spine surgery are to maximize patient function and expedite a return to an improved quality of life. As spinal surgery has evolved, more focus has been placed on minimizing trauma to the tissue during surgery, which in turn accelerates recovery through the use of minimally invasive techniques.
The era of modern spinal surgery has blossomed over the past 15 to 20 years as a result of research and technology advancements including better understandings of spinal balance, improvements in spinal implants and placement techniques, and the emergence of minimally invasive spine surgery.
These advancements have paved the way for very exciting breakthroughs in the field of computerized surgical planning, robotic-assisted surgery, and real-time spinal navigation; all of which are aimed at improving the lives of patients undergoing spine surgery. Not only will these advancements improve patient outcomes, they also improve a surgeon’s ability to understand a patient’s condition so that they can precisely plan the ideal surgical procedure and then accurately and efficiently execute that plan in the operating room.
Research is showing that by improving accuracy, patients experience better surgical results, decreased risk of complications, and less need for additional surgical procedures, all concerns for patients undergoing spinal surgeries.
Spinal & Total Body Balance
Maintaining the balance of our bodies is critical during daily activities. The human body is a series of bones and joints attached together, all stacked one on top of each other, working in the most efficient and concise manner. These structures relate to each other but are meant to be in balance.
Thinking big picture, a person’s head is meant to balance directly over their ankles when they are standing upright. Any situation that causes someone to lean forward or to the side increases stress on the body and the muscles that support it and therefore can increase pain and dysfunction of the spine. Recent advancements have put an emphasis on the importance of body and spinal balance, leading to improved surgical outcomes now that surgeons are better able to identify the necessary realignment to produce the best results.
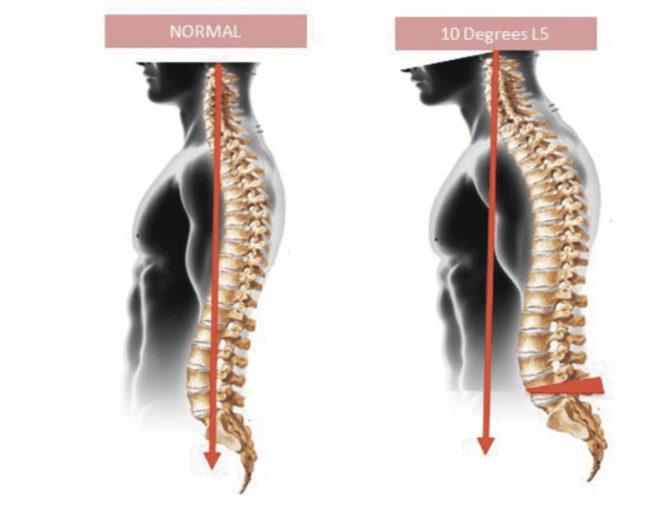
A side view of the spine with normal balance (left) and malalignment.
For example, when the spine is viewed from the side, there are multiple regional curvatures in the spine all meant to balance out so that the person’s head stays directly above their pelvis when sitting or standing. There is a normal inward curvature of the lumbar spine (lordosis) as well as a normal outward curvature (kyphosis) of the thoracic spine.
These curvatures are meant to balance out so that when standing erect, total body alignment (balance) is achieved. Any situation where one of these curvatures changes abnormally will lead to accommodations in other areas, potentially driving people out of balance. When people develop an injury, are affected by age-related degeneration, or experience an imperfect surgical procedure that drives the spine “out of balance”, their quality of life can be greatly affected by decreased function and/or increased pain.
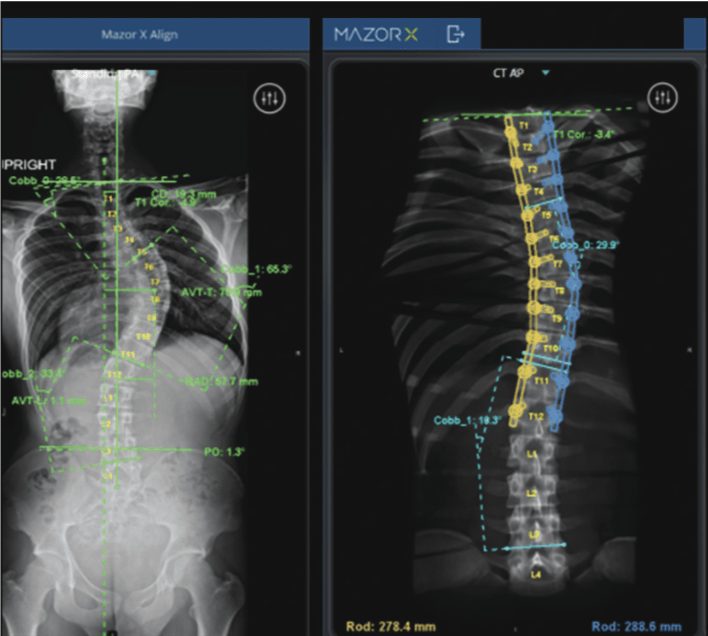
Preoperative computerized surgical plan (left) with proposed correction of spinal curvature and ideal location of implants (right).
Surgeons need to be very cognizant of optimizing a patient’s spinal alignment during any surgical procedure but especially a fusion, in which the alignment gets locked. This is where the future of computerized surgical planning becomes most important. New and evolving computer programs can allow surgeons to input multiple types of images (x-ray, CT scan, MRI scan, etc.) more challenging especially when patients have abnormal anatomy such as scoliosis or abnormal spinal curvatures where the bones are rotated. Similarly, when minimally invasive surgical procedures are being performed, the surgeon has minimal visualization of the anatomy that they are working on. Preoperative computerized planning coupled with operative robotic guidance can provide surgeons with a very powerful tool to overcome these challenges and to achieve their preoperative plan with a high degree of accuracy, ultimately improving patient safety.
Navigation in Spine Surgery
Navigation in spine surgery was first reported in 1995 and has grown significantly over time. Navigation options include using a combination of intraoperative and preoperative imaging to display real-time views of surgical tools overlapping imaging studies in the operating room. This allows a surgeon to look at the anatomy while simultaneously visualizing the imaging studies with instruments overlaid using a computerized system.
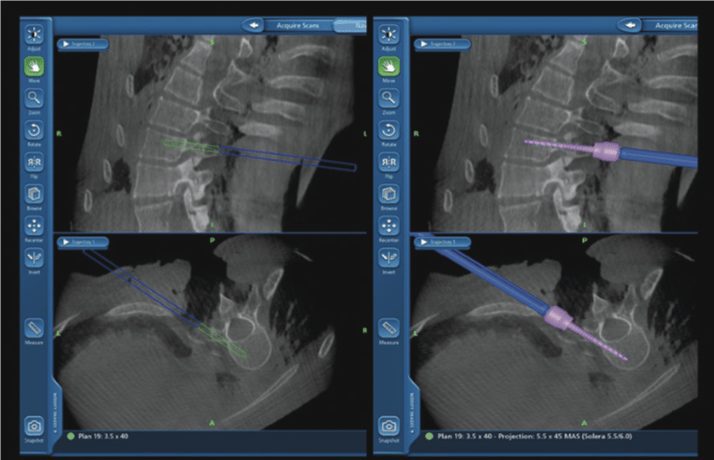
Overlay of surgical tools and implants during surgery.
Combining the patient’s own visualization anatomy with simultaneous review of the images can provide tremendous benefit. This technology is similar to using GPS guidance to travel to a desired location.
Minimally Invasive Spine Fusion
The purpose of a spinal fusion is to create a rigid union between two separate segments of the spine to correct malalignment or instability (which is a pain generator). Spine fusion has traditionally been performed using “open surgery” with an incision that is big enough to expose the entire area being treated. Open surgical techniques are beneficial and necessary for many conditions, but in some cases minimally invasive surgery (MIS) can be utilized. MIS uses smaller incisions which usually result in less damage to surrounding healthy tissue, less postoperative pain, and a faster recovery. MIS often requires an increase in the use of intraoperative x-rays in order to compensate for a surgeon’s inability to directly see the spine. In some cases, this lack of visualization decreases the surgeon’s accuracy when compared to open surgery. To compensate for the lack of visualization and to maintain accuracy, additional x-rays are required, exposing the patient and medical team to higher amounts of radiation.

Difference of incisions using a minimally invasive technique (left) vs. traditional open surgical technique (right)
Increased radiation exposure during surgery is a concern for the patient as well as the health care team as previous studies have shown an increased rate of cancer among spine surgeons than the general population.1 Robotic-guided technology and navigation allows a surgeon to precisely perform MIS while minimizing the need for radiation during surgery. Robotic technologies guide the surgeon’s tools during MIS to ensure accuracy while also decreasing tissue trauma, resulting in less bleeding, smaller scars, less pain, and faster recovery.
Robotics & Navigation Research
Studies have shown that utilizing navigation and robotic-guidance when placing implants demonstrates greater accuracy than traditional open surgery or fluoroscopic- (x-ray) guided techniques. Up until recently, almost no clinical data existed to demonstrate that this improvement in accuracy actually translates improvement in patient outcomes after surgery. The initial assumption was always that increased accuracy would lead to better outcomes through lower complications. In 2007, a meta-analysis (combination of data from multiple studies) of 130 studies with almost 40,000 spinal screws placed showed an overall accuracy rate of 91% within improvement accuracy to 95% using spinal navigation. A more recent meta analysis showing 26 prospective clinical studies with over 6,000 screws placed supported increased accuracy for screws placed and significant decrease in implant malposition with use of navigation techniques.2
Turning to robotics data, a retrospective review of over 14 medical centers with 635 cases surgeries and over 3,200 implants was published.3 They found that 98% of pedicle screws placed utilizing robotic- assisted technology was deemed to be safe and 89% to be completely contained within the bone.
In another study, 112 surgeries were retroactively evaluated and showed improvement in screw accuracy using robotics, a decrease in complication rates, and a decrease in hospital length of stay in patients treated with robotic-assisted surgery.
Another study group was formed to specifically look at patient outcomes after robotic-assisted spinal surgery with particular interest in prospectively evaluating patients undergoing fusions of the lumbar spine via a minimally invasive technique and to compare the results between patients treated with robotic-guidance versus traditional fluoroscopic techniques. The goal was to assess for differences in patient complication rates, rates of additional revision surgeries, and differences in intraoperative radiation exposure. Early results show that patients treated with robotic-guidance had a 3.1 times lower risk for a complication after a surgical procedure and a 14.7 times lower risk of needing an additional surgical procedure. There is also a 79% decrease in the amount of x-ray radiation used in the operating room for patients treated with robotic guidance.
Conclusion
Improvements in understanding total body and spinal balance are leading to improved outcomes in patients requiring spinal surgeries. Computerized preoperative planning offers a tremendous potential benefit for surgeons and patients in order to properly execute the planned spinal procedures. Robotic assistance and real-time navigation can improve the accuracy and safety of spinal surgeries and we believe these technologies will be transformative in the world of spinal surgery.